According to Nature.com, energy metabolism is the process by which cells acquire and use the energy needed to stay alive, to grow, and to reproduce. Over time disruptions in energy metabolism cause metabolic disorders.
Obesity, a disease involving an accumulation of excessive body fat, is one of the many metabolic diseases that can be caused by a person’s lifestyle, usually involving a lack of physical activity, combined with environmental factors, like unhealthy food intake, and possibly genetic factors. In recent decades, it has become a significant health issue, seeing an increase across the world at an alarming rate. One major physical aspect that is adversely affected by obesity is reproductive health.
There are many studies that hypothesise the links between energy metabolism and fertility in animals. In birds and mammals, an energy deficit can be sensitive to the reproductive system. For instance, it’s been reported that food restriction in prepubertal female rats prevents the normal onset of puberty. In pigs, a negative energy balance and a decrease in body fat result in a reduction in litter size and viability of piglets.
In humans, however, experimental and clinical studies have revealed that obesity has negative impacts on male and female reproductive functions. Obese women have been known to face higher rates of complications in their pregnancy, including gestational diabetes and rates of cesarean delivery.
PCOS
Obesity is closely linked with Polycystic Ovary Syndrome (PCOS), an endocrine-metabolic disorder causing enlarged ovaries with small cysts on the outer edges. Women with PCOS produce higher amounts of the male hormone androgen, more than the normal range. The exact cause of polycystic ovary syndrome isn’t well understood but may involve a combination of genetic and environmental factors. Symptoms include menstrual irregularity, excess hair growth, acne and obesity.
PCOS is often correlated with profound insulin resistance as well as with defects in insulin secretion. Insulin resistance occurs when cells in your muscles, fat, and liver don’t respond well to insulin and can’t utilise glucose from your blood for energy. To make up for it, your pancreas generates more insulin. Over time, your blood sugar levels go up. The insulin resistance in at least 50% of women suffering from PCOS seems to be related to excessive serine phosphorylation of the insulin receptor. Serine phosphorylation modulates the activity of the key regulatory enzyme of androgen biosynthesis, leading to both insulin resistance and hyperandrogenism (androgen is a male hormone) in some PCOS women.
It is also found to be more marked in obese women, suggesting that PCOS and obesity have a synergistic effect on the extent of the insulin disorder. Hyperinsulinemia, essentially a higher than normal level of insulin in your blood sugar, is associated with insulin resistance and has been causally connected to all features of PCOS, such as hyperandrogenism, reproductive disorders, acne, hirsutism, and metabolic disturbances.
Energy Metabolism and infertility in Women
In female animals, studies have observed that reproduction and metabolism are tightly connected and reciprocally regulated. The activity of the reproductive system, with their cyclic production of hormones, ensures a continuous regulation of energy metabolism.
In female mammals, in particular, energy metabolism is focused on reproductive needs—the energy spent on puberty, pregnancy and lactation rely on the female’s ability to save and conserve energy. Evolution has ensured that there are mechanisms in place to store energy in case of abundance in food and to prevent reproduction in case of lack of food or poor nutrient environments. The disruption in the harmony between reproduction and metabolism is when problems occur. For instance, physiologically, after menopause, women are at a higher risk of developing metabolic and cardiovascular disorders.
Nature’s gender-specific strategy developed for survival over the course of thousands of years now has negative effects on female health and fertility, owing to the modern obesogenic world.
The link between metabolism, obesity and reproductive health is becoming clearer as more cases across the world are being studied.
Infertility, for example, is so rampant nowadays in both men and women that it affects one in seven couples, with the numbers only rising. A large number of these cases are directly or indirectly related to obesity.
A strong relationship has been observed between decreased insulin sensitivity and infertility in diabetic and women with PCOS, indicating that the amount and quality of carbohydrates in the foods they consume may affect and influence female reproductive functions.

Energy Metabolism and infertility in Men
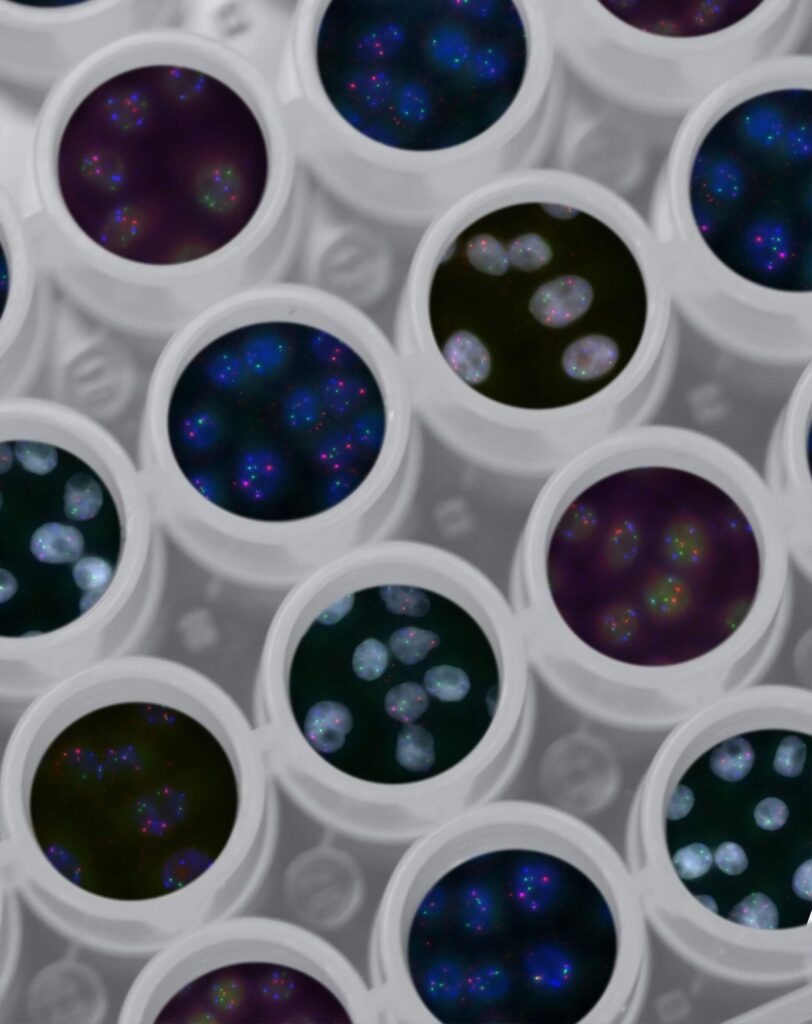
Energy metabolism is known to play a key role in men’s health, wherein the reproductive system is affected when metabolism fluctuates. Men who are obese can have decreased sperm quality, sperm concentration, sperm motility, acrosome reaction decline, increased sperm DNA damage, and lower embryo implantation rates, compared to men with normal BMIs, according to clinical studies.
How does Energy metabolism affect testosterone?
Testosterone is a major hormone in both men and women. In men, it is produced mainly by the testicles. It affects a man’s appearance, giving him male features like body/facial hair, a deeper voice, etc., and his sexual development. It is key to a man’s sex drive and sperm production. Its other contributions include building muscle and bone mass. Low testosterone levels in men can cause a range of issues such as:
- Low sex drive
- Irregular erections
- Reduced semen volume
- Hair loss
- Fatigue
- Changes in body composition
In the year 2010, the endocrine society clinical practice guidelines recommended that men with type 2 diabetes should be screened for low testosterone levels. Studies have also reported that obese men with type 2 diabetes can possibly have secondary hypogonadism because of peripheral and central insulin resistance. Hypogonadism is a condition in which the body produces lower than normal levels of testosterone or normal sperm production or both. In secondary hypogonadism, the testicles are normal but don’t function properly due to a problem with the pituitary gland or hypothalamus.
In obese men, SHBG (sex hormone-binding globulin)—a protein responsible for transporting hormones like testosterone to the blood—is reduced as a result of increased insulin levels in circulation, associated with the insulin levels of obesity. However, after adjusting for the SHBG levels, studies found that low testosterone levels are shown to be correlated to insulin resistance and obesity. This denotes an independent effect of insulin resistance on testosterone production and male fertility.
Conclusion
The ubiquity of overweight and obese men and women in some developed countries has gone beyond 50%. It is also increasing worldwide, thereby increasing the associated risks. It is also linked clearly to many reproductive disruptions in women, including anovulation, subfertility, infertility, increased risk of miscarriage and poor neonatal and maternal pregnancy, and men, resulting in erectile dysfunction, poor semen quality and subclinical prostatitis. It is imperative that blood sugar levels and risks of obesity be monitored regularly to avoid any chances of poor reproductive functioning.