Your nervous system plays a massive role in how your body processes energy, handles blood sugar, and responds to stress. At the center of it all is the vagus nerve. (PMID: 10647058)
The vagus nerve connects your brain to key metabolic organs like the pancreas, liver, gut, and fat tissue. You can read our full guide to the vagus nerve and how it affects heart rate variability.
And it doesn’t just relay information. It actively helps regulate inflammation, glucose levels, insulin sensitivity, and more. When your vagal tone is strong, your metabolic system becomes more resilient. When it’s weak, stress and inflammation take the lead.
Here’s what you need to know about how the vagus nerve shapes metabolic health, the studies that prove the link, and how you can take control.
Your metabolism runs on signals from your brain
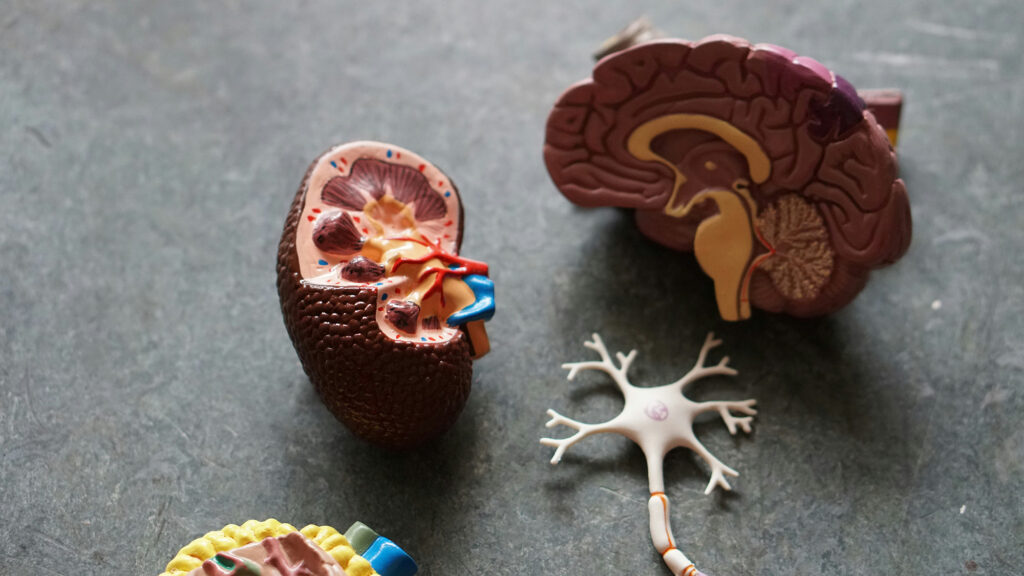
The vagus nerve is the tenth cranial nerve. It starts in your brainstem and extends into the heart, lungs, liver, pancreas, gut, and more.
80% of its fibers send information from your body to your brain (afferent). The other 20% deliver instructions from the brain to the body (efferent).
And it plays key roles in the gut, pancreas, and liver.
- In the gut, it helps regulate satiety and appetite.
- In the pancreas, it supports insulin release after eating. (PMID: 20716695)
- In the liver, it helps coordinate glucose storage and production. (PMID: 10647058)
When vagal tone is strong, these systems communicate efficiently. Blood sugar stays stable. Energy use is balanced.
Stimulating the vagus nerve can improve glucose control
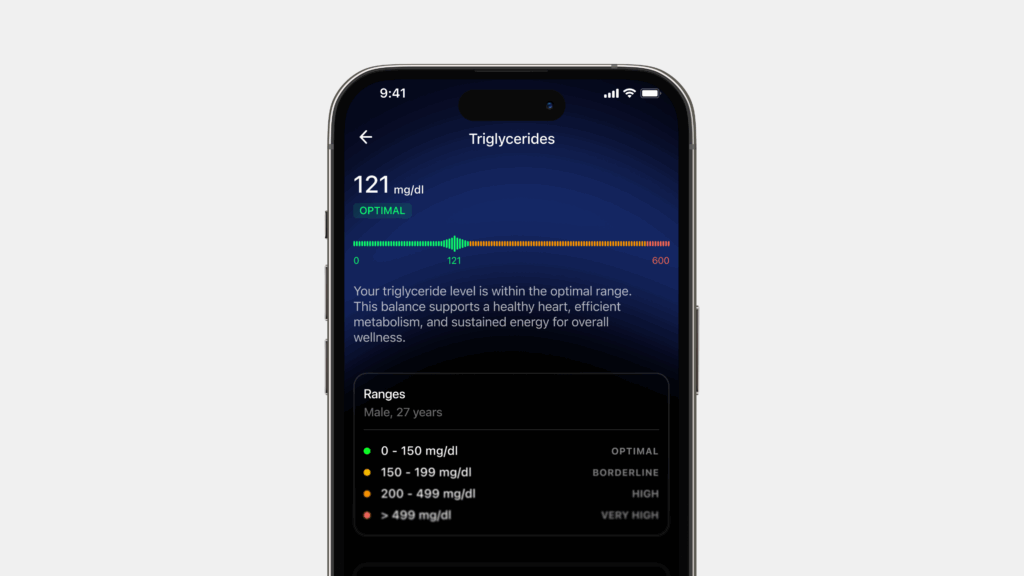
If your vagus nerve isn’t working well, your tissues may become less responsive to insulin. This is called insulin resistance, a key driver of metabolic dysfunction.
Animal studies have shown that stimulating the vagus nerve can restore insulin sensitivity and improve glucose uptake in muscle and liver, even without major weight loss. (PMID: 37397461)
This suggests that improving vagal tone could help your body use insulin more effectively – a big deal if you’re trying to prevent or manage type 2 diabetes.
What you can do: Read our list of 10 ways to boost HRV.
Why vagal tone and HRV affect glucose control
Chronic stress ramps up your sympathetic nervous system (fight or flight mode) and pushes your body toward inflammation and fat storage. If your vagal tone is low, you can’t shift gears back into rest-and-digest mode easily.
This can lead to:
- Poor glucose control
- Increased visceral fat
- Elevated cortisol
HRV is often lower in people with insulin resistance and type 2 diabetes (PMID: 8861461). That’s not a coincidence. A more responsive vagus nerve = better metabolic control.
How to stimulate the vagus nerve
You don’t need expensive devices or clinical interventions to support your vagus nerve. There are simple, proven ways to stimulate it that can improve glucose control, reduce inflammation, and enhance metabolic flexibility. Here are the most effective, science-backed strategies.
1. Resonance breathing
- What it is: Slow, deep breathing at a rate of 4.5 to 6 breaths per minute.
- Why it works: Activates baroreceptors that enhance vagal tone and improve heart rate variability.
- How to do it: Inhale for 5 seconds, exhale for 5 seconds. Repeat for 5–10 minutes daily.
2. Cold exposure
- What it is: Cold exposure to the face or neck, or full-body cold showers.
- Why it works: Stimulates the mammalian diving reflex, increasing parasympathetic activity.
- How to do it: Splash cold water on your face or end your shower with 30–60 seconds of cold water.
3. Hum
- What it is: Humming, singing, gargling.
- Why it works: Engages muscles connected to the vagus nerve, especially in the throat and vocal cords.
- How to do it: Hum or gargle loudly for 30 seconds daily. Singing works too.
4. Eat probiotic
- What it is: Foods that support gut bacteria, like yogurt, kefir, sauerkraut, garlic, and oats.
- Why it works: A healthy gut enhances vagus nerve signaling via the gut-brain axis.
5. Get good sleep and rest
- What it is: Consistent sleep, stress management, and time for recovery.
- Why it works: Poor sleep and chronic stress suppress vagal tone and promote inflammation.
- How to do it: Aim for 7–9 hours of quality sleep. Avoid screens and heavy meals before bed.
These strategies may seem simple, but they train the vagus nerve consistently over time – and that consistency is what helps shift your metabolic system from reactive to resilient.
Summary
There’s strong evidence that the vagus nerve has an influence over the way our bodies process food for energy, and our blood sugar levels.
If you want better metabolic health, better glucose control, and more energy balance, supporting your vagus nerve, combined with diet, exercise, and good metabolic habits, could be an important tool in managing glucose and maintaining a healthy weight.