When most people think about the menstrual cycle, they think of periods, ovulation, or conception. But the truth is: your cycle is much more than that. It’s a beautifully complex interaction of anatomy, hormones, and processes – all working together to prepare the body every month.
And here’s something you may not know: the menstrual cycle isn’t a single cycle at all. It’s actually two cycles running side by side – the ovarian cycle and the uterine cycle.
The four stages of the menstrual cycle – and how you might feel
Together, they’re regulated by five major hormones: three that originate in the brain (gonadotropin-releasing hormone or GnRH, follicle-stimulating hormone or FSH, and luteinizing hormone or LH) and two from the ovaries (estrogen and progesterone).
These hormones connect the brain, ovaries, and uterus through an intricate feedback loop, ensuring that every month, the body has the potential to conceive – or reset and prepare again.
But the cycle’s impact doesn’t stop at reproduction. Each phase leaves its own unique “fingerprint” on your physiology: shifts in body temperature, changes in heart rate, differences in energy and recovery. By learning to read these patterns, you can understand your body’s rhythms more deeply – helping you decide when to train harder, when to eat for fuel, or when to give yourself rest.
Breaking down the phases of the uterine cycle

The menstrual cycle exists as part of the female body’s reproductive preparation system. Typically, it’s a monthly biological rhythm that gets the uterus ready for a possible pregnancy and ensures an egg is available for fertilization. Those day ranges describe a typical 28-day cycle; many people’s cycles are longer, shorter, or variable, and phase days can shift. This moving story is written in hormones and signals. Let’s walk through the phases.
The menstrual flow – typically days 1 to 5
The prominent marker of the menstrual cycle is the menstrual flow, which typically recurs every 21 to 35 days. It begins when no fertilized egg implants at the end of the previous cycle. As a result, the uterus sheds its inner lining (the endometrium) in a process we call menstruation, or “menses.” It’s accompanied by bleeding through the vagina.
In this phase, your hormone levels (particularly estrogen and progesterone) are at their lowest, often leaving you feeling lower in energy or mood. It’s also when many people experience cramps, bloating, or fatigue. The bleeding might be light or heavy, painful or less so, long or short. Typically, it lasts between 2 and 7 days. The shedding clears the way for a fresh cycle.
The proliferative phase – typically days 5 to 13
Once menstruation ends, the proliferative phase begins in the uterine cycle. Under the influence of rising estrogen, the uterine lining starts to rebuild and thicken. Blood vessels and tissue grow, creating a nutrient-rich foundation for a possibly fertilized egg. This growth phase lays the groundwork for the uterine environment, even as events unfold in the ovaries.
The rising estrogen levels make you feel more energetic. Your mood starts to lift.
Running in parallel is the follicular phase of the ovarian cycle, typically days 1 through 13. Stimulated by follicle-stimulating hormone (FSH), the ovaries begin developing multiple follicles, each housing an immature egg. As estrogen levels climb, usually only one follicle fully matures and pushes toward the ovarian surface.
Ovulation – typically around day 14
Mid-cycle, typically around day 14, a sharp surge of luteinizing hormone (LH) causes the mature follicle to rupture. The egg is released into the fallopian tube and begins its journey toward the uterus. If sperm are present, fertilization can occur. If not, the egg will simply dissolve, and the cycle moves forward.
Ovulation can influence basal body temperature, cervical mucus consistency, and sometimes even libido or energy levels. Many women experience pelvic pain or cramping during ovulation.
The secretory phase – typically days 15 to 28
The uterine cycle prepares for a fertilized cell, entering the secretory phase. The endometrium’s glands enlarge, secrete nutrient-rich substances, and increase blood supply, which makes the uterus highly receptive to an implanting embryo. It is supported by the ovarian cycle. The dominant unsuccessful follicle ruptures and transforms into the corpus luteum, a temporary hormone-secreting structure that produces progesterone and estrogen.
Some women also feel more tired or have trouble sleeping during the luteal phase, since higher progesterone levels can affect energy and sleep.
As the uterine lining starts to break down, progesterone and estrogen levels fall. It often leads to common premenstrual symptoms like mood swings, headaches, acne, bloating, and breast tenderness.
When progesterone and estrogen drop, the cycle begins again.
Beyond reproduction: your cycle as a health signal
The menstrual cycle isn’t just about reproduction – it’s one of the body’s most important rhythms. Each stage can affect your:
- Energy and training capacity: You might feel more powerful in the follicular phase, and need more recovery in the luteal phase.
- Mood and sleep: Estrogen and progesterone fluctuations can shift sleep quality, anxiety, and resilience.
Many studies show subtle but consistent signals in biomarkers, for example, a post-ovulatory rise in basal/core body temperature, small increases in resting HR, and decreases in vagally mediated HRV in the luteal phase – though magnitudes vary across people and measurement methods. By learning to observe these signals, you can align workouts, nutrition, and rest with your body’s natural rhythm – rather than working against it.
The challenge of tracking cycles
Here’s the catch: not everyone has a textbook 28-day cycle. In fact, research shows that about 87% of women don’t. Cycles can vary in length, ovulation timing can shift, and conditions like PCOS or endometriosis can make tracking even more complex.
Traditional apps often assume regularity, predicting ovulation based on averages rather than your actual physiology. That’s why so many people find cycle tracking unreliable – and why an evidence-based, personalized solution is needed.
Enter Ultrahuman’s Cycle & Ovulation Pro
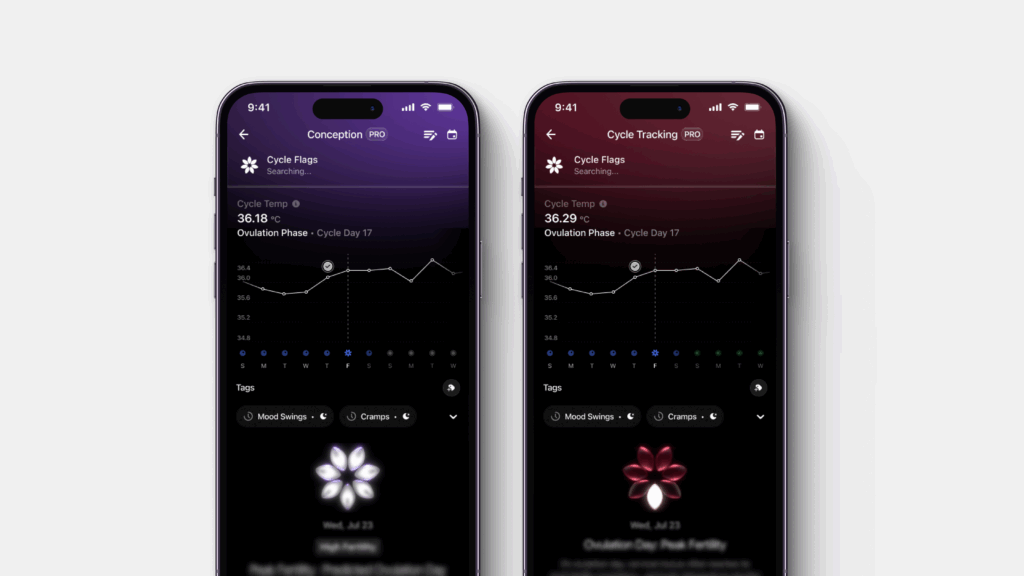
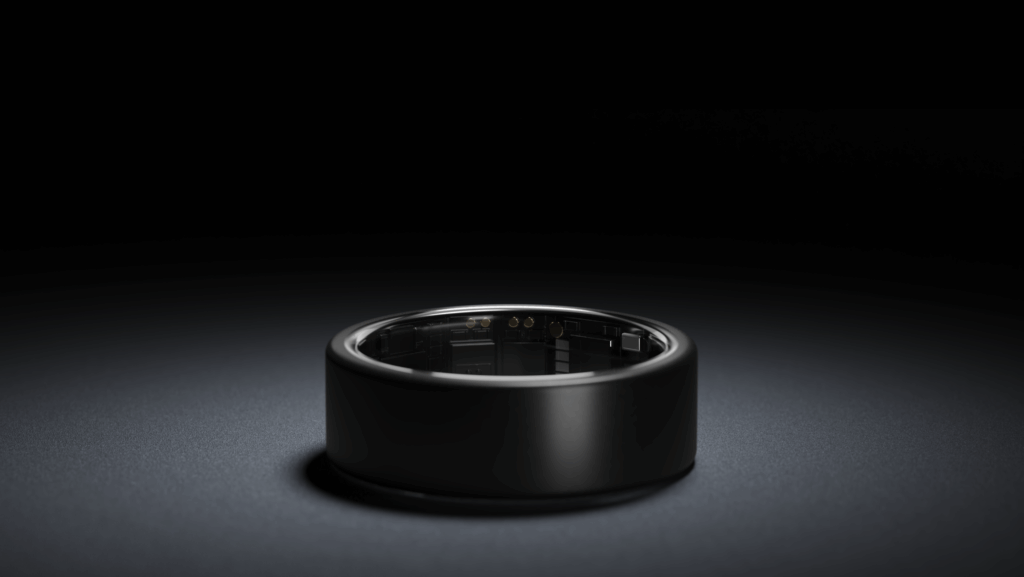
Ultrahuman’s Cycle & Ovulation Pro uses the clinically validated OvuSense™ algorithm, integrated with the Ring AIR, to track cycles with over 90% accuracy in confirming ovulation.
Beyond timing, it can reveal patterns such as delayed ovulation, short luteal phases, or signals that may indicate conditions like PCOS or thyroid imbalances. By allowing symptom and lifestyle tagging, it helps connect daily experiences with biological data for a fuller picture of cycle health.
With continuous biomarker tracking through the Ring AIR, the approach offers a seamless, science-backed way to understand the body’s monthly changes. Because your cycle isn’t just a calendar event – it’s a data-rich rhythm, and with the right tools, it can become your strongest ally.
References
- Reed BG, Carr BR. The Normal Menstrual Cycle and the Control of Ovulation. [Updated 2018 Aug 5]. In: Feingold KR, Ahmed SF, Anawalt B, et al., editors. Endotext [Internet]. South Dartmouth (MA): MDText.com, Inc.; 2000-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279054/
- Ultrahuman blog: https://blog.ultrahuman.com/blog/four-phases-of-the-menstrual-cycle/
- Mayo Clinic post: https://www.mayoclinic.org/healthy-lifestyle/womens-health/in-depth/menstrual-cycle/art-20047186
- Thiyagarajan DK, Basit H, Jeanmonod R. Physiology, Menstrual Cycle. [Updated 2024 Sep 27]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK500020/
- Ecochard R, Bouchard T, Leiva R, Abdulla S, Dupuis O, Duterque O, Garmier Billard M, Boehringer H, Genolini C. Characterization of hormonal profiles during the luteal phase in regularly menstruating women. Fertil Steril. 2017 Jul;108(1):175-182.e1. Epub 2017 Jun 1. PMID: 28579410.
- Baker FC, Siboza F, Fuller A. Temperature regulation in women: Effects of the menstrual cycle. Temperature (Austin). 2020 Mar 22;7(3):226-262. PMID: 33123618; PMCID: PMC7575238.
- Schmalenberger KM, Eisenlohr-Moul TA, Jarczok MN, Eckstein M, Schneider E, Brenner IG, Duffy K, Schweizer S, Kiesner J, Thayer JF, Ditzen B. Menstrual Cycle Changes in Vagally-Mediated Heart Rate Variability are Associated with Progesterone: Evidence from Two Within-Person Studies. J Clin Med. 2020 Feb 25;9(3):617. PMID: 32106458; PMCID: