For a long time, the HbA1c test, conducted in a lab, was hailed as the gold standard for measuring blood sugar. There’s a new metric in town that can help to track glucose levels and overcome some of the limitations of the former parameter. It’s called Time in Range.
This measure originates from the world of continuous glucose monitoring (CGM) devices and can deliver live data about blood sugar to users. It offers several advantages – like keeping track of high and low blood sugar (hyperglycemia and hypoglycemia), seeing one’s cause-and-effect patterns through behaviour, and its impact on glucose. Seeing data for blood sugar impact our daily actions helps us make behaviour changes as they occur. It can nudge us into maintaining steady blood sugar levels.

Highlights
- Time In Range is a count for the percentage of time a person spends within their blood glucose levels in a target range,
- The range will vary depending on the person, but general guidelines suggest starting with a range of 70 to 110 mg/dL,
- Blood glucose in terms of time in range offers a more nuanced, cause-and-effect understanding of blood sugar levels. An optimised TIR can lead to enhanced metabolic health.
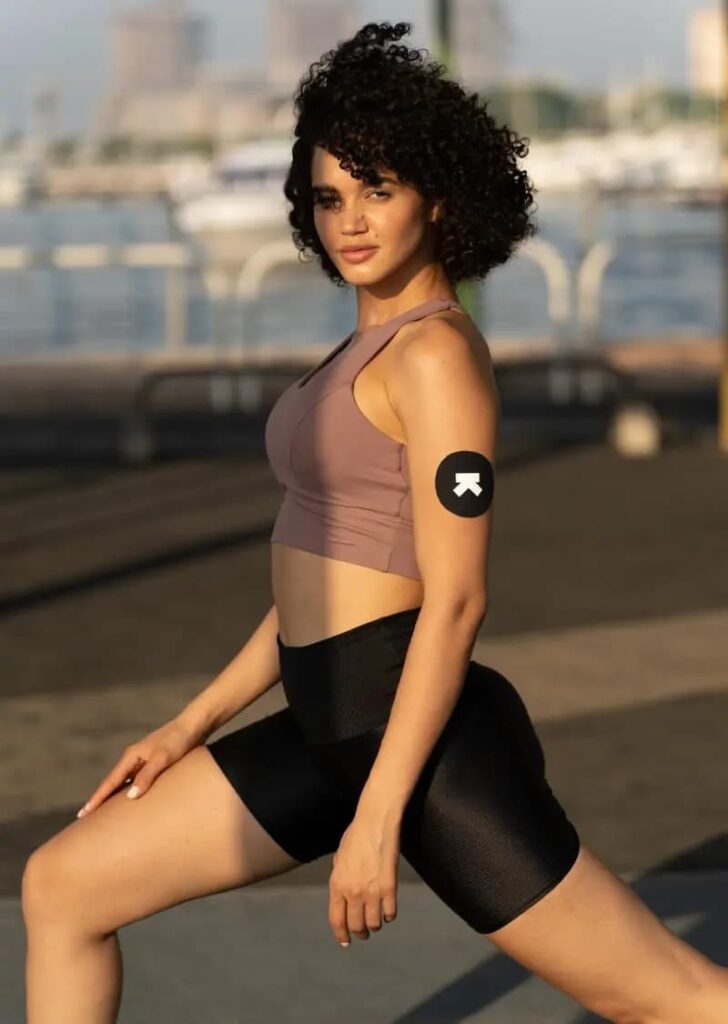
A CGM device deploys a tiny sensor that can be inserted under the skin, usually on the upper arm or abdomen and assesses blood sugar levels in the interstitial fluid. The measures are displayed instantaneously on the user’s phone. On the other hand, the glucose monitor test can measure your blood sugar levels one pinprick at a time.
What is Time in Range?
For people tracking their glucose levels, the measure of Time in Range (TIR) can simplify matters. TIR measures how much time one’s blood glucose levels have been in a healthy target range. It is defined as “the percentage of time spent at or above the lower boundary (70 mg/dL) and below or equal to the upper boundary (180 mg/dL) during a specified period.” For a suitable TIR count, one must maintain balanced blood glucose levels – enabled through timely data, an understanding of one’s body, and decisiveness to responsively alter one’s lifestyle.
The scope of behaviours that impact blood sugar typically involves diet choices, medicative actions, and even exercise. Higher the time spent in the normal range, the better the CGM user’s glycemic/glucose control.
The period during which one’s glucose levels are within this normal range is called bright spots and when the person’s levels are out-of-range, the instances are referred to as landmines.
Importance of Time in Range
A helpful feature of Time in Range (TIR) as a measure is how it accounts for hypoglycemia, ie, low blood sugar levels. These are thought to be as detrimental as high blood sugar levels, if not more. HbA1C testing has been a norm for glucose levels, though it does not measure hypoglycemia.
However, with a CGM device, it is simple to measure hypoglycemia through TIR. Research also lends credence to a strong correlation between the time spent out-of-range and susceptibility to diabetes complications.
An HbA1C test captures the average of one’s glucose levels over 2-3 months. Its results provide a big-picture view of how your body is handling glucose. An HbA1C level between 5.7% and 6.4% are classified as pre-diabetes.
Anything at 6.5% or above indicates diabetes. As this test shows an average over a long period of time, its trade-off is the details of frequent and natural volatility of blood sugar in one’s daily life.
On the other hand, TIR tracking allows access to real-time blood sugar data. It also highlights the duration of blood sugar levels in the optimal range and the duration and intensity of any diversions.
It can provide actionable insights to carry out small yet impactful lifestyle changes and regulate your blood sugar levels. As the user logs in their meals, mealtimes and activity, they can check their TIR.
This can help them understand the particular foods that spike their blood sugar vs the ones that steadily release glucose in the bloodstream, the activity that flattens their blood glucose curves, the ideal time to exercise and fuel up, the impact of stress and sleep on blood glucose levels and more. Doctors still recommend A1C testing in conjunction with TIR tracking for a well-rounded approach to your care.
How Staying Out of Range can Negatively Affects Your Metabolism?
There are risks that arise from hypoglycemia (low blood sugar) as well as hyperglycemia (high blood sugar). With low blood sugar, one risk is that it can escape undetected, leading to the body producing fewer symptoms over time as well.
Individuals with hypoglycemia unawareness can’t tell when their blood sugar plummets so they don’t realise that they need to address it. The risks include a loss of consciousness, a seizure and even death.
It can also be a contributing cause of conditions like dizziness, falls, injuries, weakness, and accidents from a lack of awareness. It increases the risk of dementia in older adults.
The TIR measure through a CGM is an effective way of monitoring this and taking corrective measures.
On the other hand, hyperglycemia or high blood sugar manifests in symptoms such as blurry sight, frequent urination, headaches, and a higher appetite for food and drink. It can also lead to fatigue, skin and vaginal infections, weight loss, and cuts or sores healing slowly.
Under type 1 diabetes, high blood sugar can develop into a condition called ketoacidosis, which is considered a medical emergency.
Symptoms of ketoacidosis are dehydration, deep breathing or hyperventilation, a sense of disorientation or confusion from the environment. In certain extreme cases, ketoacidosis can cause a coma or even death.
Nondiabetic hyperglycemia refers to blood glucose (sugar) elevation in the absence of diabetes.
Research suggests that postprandial or post-meal blood sugar spikes in non-diabetic people are risk factors for cardiovascular disease and insulin resistance, markers of metabolic dysfunction.
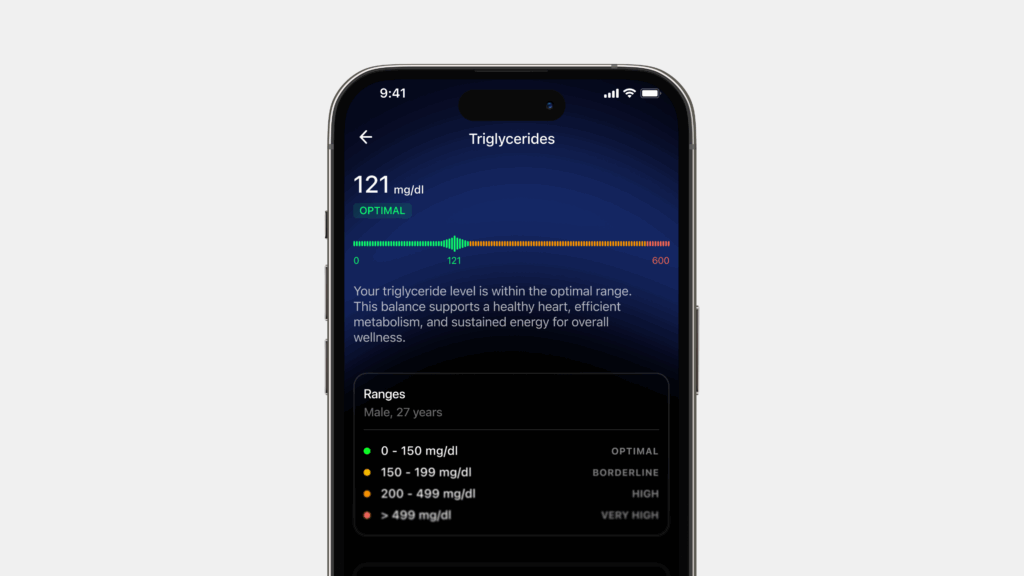
Staying in range with the TIR metric can help one regulate their post-meal hyperglycemia. This brings us to the concept of metabolic health. It refers to ideal levels of triglycerides, HDL cholesterol, blood pressure, blood glucose levels and waist circumference, without the intake of medication.
A good way to keep track of metabolic health is through the measure of glycemic variability.
It refers to blood glucose fluctuations including hypoglycemic phases and postprandial rises, as well as blood glucose swings that occur at the same time on different days.
Our glucose levels oscillate throughout the day naturally. It’s the extent of the swaying that matters. The lower the TIR, the higher the glucose variability.
Simply put, glycemic variability measures the fuel (whether fat or glucose) quality and oxidative stress imbalance between reactive oxygen and antioxidant defences) in your body.
Keeping your blood glucose variability under 12% is a good goal to have. Free radicals are extremely reactive and fight pathogens, which can cause infections.
Antioxidants stabilise their reactive nature and create functional harmony. Sharp changes in blood sugar levels can cause oxidative stress and cause cellular damage. Oxidative stress is associated with inflammatory diseases like cancer and Alzheimers.

Benefits of the Time in Range Metric for Tracking Blood Glucose Level
According to this study, there are several benefits of using TIR. These include:
- A person can keep a valid score of how daily activities like food, exercise, and sleep habits impact blood glucose in real-time. Such data shows clear and live cause and effect. Armed with such intel, one can improve their lifestyle through behavioural choices,
- Healthcare professionals can offer a higher degree of customised care to support people. As not all bodies react the same way to such behaviours, the variance and inter and intra-day differences can be documented,
- As the market for TIR evolves, one may save money on A1C tests while getting a more timely and relevant reading by this mechanism,
- Time in Range is a clear, simple measure for glucose levels that one can understand and navigate by themselves.
Ideal Time in Range for Tracking Optimal Glucose Level
Glucose levels fluctuate over the course of one’s day, so it’s expected to see a curve with moderate peaks and valleys. However, the ideal measure is 100% TIR (which translates to all 24 hours).
Blood Glucose Optimal Range to Target
People aiming for optimal metabolic health should target a blood sugar range of 70 to 110 mg/dL for as much of the day as possible.
According to the American Diabetes Association (ADA), people can be categorised into three categories based on fasting glucose levels: normal, prediabetes, and diabetes.
Fasting glucose must be under 100 mg/dl to be regarded in the normal range. When the fasting blood sugar level is greater than or equal to 126 mg/dl, it is considered to be a diagnosis of diabetes.
The International Diabetes Federation (IDF) suggests that nondiabetic people should not have a glucose level of higher than 140 mg/dl after meal consumption, and glucose should return to pre-meal levels within 2-3 hours.
Research is still progressing to form universally accepted standards for what “normal” 24-hour glucose values should be. CGM technology can be an essential tool in furthering such research.
Optimal glucose levels using a CGM depend on individual health goals and are to be discussed with one’s healthcare/nutrition consultant. These measures are worth considering as broad targets and may apply to your personal condition, situation, or goal.
It is always recommended to consult a medical professional about the right TIR goals for you, which can shift for a variety of reasons, including if you’re pregnant, older, or at high risk of complications.
How to Improve My Time in Range to Monitor Glucose Level?
- Check blood sugar levels consistently and frequently, and use the data to understand your patterns
- Minimise the sharpest blood sugar spikes and correct their causes — such as too many carbohydrates at one time or being sedentary after meals.
- Correct a pattern of glucose drops with a nutrition consultation.
- Make course corrections when out-of-range blood sugars occur with steps like post-meal walks or adopting the appropriate fueling strategy.
- Identify and replicate Bright Spots—when you have a day with lots of TIR, what happens? How can you replicate those decisions?
- Build routines to minimise actions that cause upheaval in blood sugar—when you are not in the target range, what choices drove that? How can you avoid those decisions next time?
Conclusion
Time In Range is a count for the percentage of time a person spends within their blood glucose levels in a target range. The range will vary depending on the person, but general guidelines suggest starting with a range of 70 to 110 mg/dL.
Because Time in Range glucose can be measured at home on a daily or weekly basis, it has a huge advantage over HbA1C: understanding what behaviours and choices prompt more TIR (Bright Spots), what drives out-of-range blood glucose levels (Landmines), and where/when changes can be made (e.g. time of day).
Thinking about blood glucose in terms of time in range offers a more nuanced, cause-and-effect understanding of blood sugar levels than A1C. An optimised TIR can lead to enhanced metabolic health.
Keep in mind: These are just targets, so they aren’t personalized to your specific situation. You should always consult a medical professional about the right TIR goals for you, which can shift for a variety of reasons, including if you’re pregnant, older, or at high-risk of complications.
Disclaimer: The contents of this article are for general information and educational purposes only. It neither provides any medical advice nor intends to substitute professional medical opinion on the treatment, diagnosis, prevention or alleviation of any disease, disorder or disability. Always consult with your doctor or qualified healthcare professional about your health condition and/or concerns and before undertaking a new healthcare regimen including making any dietary or lifestyle changes.
References
- https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-020-00529-z
- https://www.health.harvard.edu/blog/is-blood-sugar-monitoring-without-diabetes-worthwhile-202106112473
- https://pubmed.ncbi.nlm.nih.gov/30575414/
- https://pubmed.ncbi.nlm.nih.gov/28541136/
- https://care.diabetesjournals.org/content/31/10/2072