Glucose is a major source of energy for the cells and one of the most important molecules in the body. Disruptions in glucose levels or the way in which the body processes glucose can lead to various health problems since it is linked to the most dominant bodily functions. Glucose regulation is tied to metabolic health. Monitoring glucose levels can offer insights into our health as well as have benefits in terms of implementing changes in lifestyle, diet, or exercise.
Highlights
- Blood sugar levels fluctuate all day long. Patterns of rises and crashes can offer valuable and actionable insights into your metabolic health,
- The burning of fat is closely tied to insulin levels, which in turn depend on, or are closely related to, blood glucose,
- A good first step is becoming aware of where your levels stand. Glucose monitoring can provide you with great insights such as glucose variability.
The body produces glucose from protein, fat, and, most frequently, carbohydrates. It is a simple sugar or monosaccharide. Glucose is absorbed directly into the blood from the intestines, which results in a rapid increase in blood glucose or blood sugar. It is then transported through the bloodstream to generate energy for all the cells in the body. Our cells cannot use glucose without the help of insulin, a hormone that allows cells to absorb it. Thus, the body depends on glucose to keep all its mechanisms functioning effectively, giving us the energy to go about our day-to-day activities.
Glucose levels often go unnoticed when they are within the ideal range. However, when these levels in the blood are too high or low, our normal functioning is affected. There is a complex system in place for keeping glucose within a healthy range, metabolizing it into fuel, or storing it for later use. Insulin plays a crucial role in this process.
How to Monitor Blood Glucose Levels?
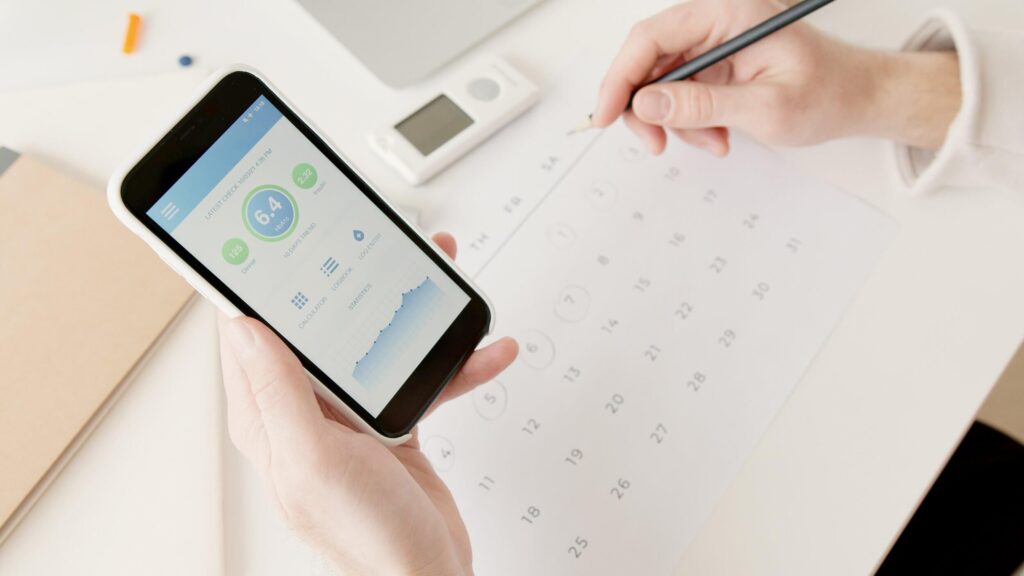
By tracking the metabolic biomarker of glucose levels, it is possible to understand what kinds of foods or activities are helpful in glycemic control. Blood sugar levels fluctuate all day long.
Patterns of rises and crashes can offer valuable and actionable insights into your metabolic health.
There are a number of tests that can help you understand your blood sugar the A1C test, measures your average blood sugar levels over the past two or three months.
The fasting blood sugar test measures blood sugar after not eating overnight, and the glucose tolerance test, which measures blood sugar levels after ingesting a glucose-containing liquid and also checks the post-meal glucose levels. However, the most accurate measure of glucose over time can be done by continuous glucose monitoring (CGM), which automatically tracks blood glucose levels around the clock.
You can check your glucose level anytime at a glance, and can also observe how it changes over the course of a few hours, days, or weeks to notice patterns. CGM works through a tiny sensor inserted beneath your skin, usually on your belly or arm. The sensor measures your interstitial glucose level, which is the glucose found in the fluid between your cells.
The sensor tests glucose at regular intervals, every few minutes. A transmitter wirelessly sends this information to a monitor, which may be part of an insulin pump or a different type of device, where your sugar level is displayed every 1, 5, 10, or 15 minutes. Your monitor will sound an alarm if your sugar drops to a dangerously low level or a high preset level.
Six benefits of monitoring blood glucose levels
You can keep your blood glucose levels at an optimum range in a number of ways. A good first step is becoming aware of your glucose levels and the pattern of dives and rises. By identifying and recording changes in blood glucose levels over time, you can see how different foods, workouts, or other factors can affect them, and this can lead to improvements in metabolic health.
Glucose monitoring can give you great insights into constructs like glucose variability, which represents the quality of fuel and oxidative stress on your body. Optimising blood glucose levels through regular monitoring can have various benefits in terms of controlling metabolism, managing weight, understanding your ideal diet, and improving athletic performance.
1.Understanding Glycemic Variability
Glycemic variability represents the quality of fuel and oxidative stress on your body. Keeping your blood glucose variability under 12% is considered ideal. Oxidative stress is defined as a disturbance in the balance between the production of reactive oxygen species (free radicals) and antioxidant defences. Free radicals fight pathogens that provoke infections. They are extremely reactive, while antioxidants stabilize the reactive nature of free radicals, creating harmony.
2.Weight Loss and Glucose Monitoring

(Image credits: Favorece)
The process of gaining or losing weight is linked with many hormonal pathways and it is not as simple as the mere movement of calories in and out of one’s body, because different individuals can have variable glucose responses to the same foods or caloric intake.
In fact, the burning of fat is closely tied to insulin levels, which in turn depend on, or are closely related to, blood glucose. Real-time glucose measurements can help us to analyse the ways in which what we eat can affect our blood sugar levels and, by proxy, our insulin levels.
Insulin is the body’s main anabolic hormone, meaning it promotes the storage of fat rather than breaking compounds down. Insulin enables our cells to take up glucose from the blood for use, or, when there’s excess, for storage. Because weight loss generally requires us to burn this stored glucose (in the form of fats), we need to control insulin, to indicate to the body that it needs to burn fat rather than store more of it.
Monitoring our glucose levels can help us to manage that, and also provide a valuable understanding of the physiological processes that lead to glucose storage or weight loss.
3.Diet and Glucose Monitoring
Diet is the most significant determinant of our blood glucose levels. Viewing diet through the lens of blood glucose levels can be a transformative technology when it comes to personalizing food choices and optimizing overall metabolic health. The same foods can have very different glucose responses for different individuals and, thus, monitoring these responses can help to create a diet plan that is optimized for your body type.
The main goal of monitoring is to ensure that glycemic variability is not too high. Glycemic variability is defined as the range of swings in glucose levels. Research suggests that excessive peaks and dips in glucose can lead to damaging effects on our metabolic health and increased risks to cardiovascular health and the nervous system.
Although the glycemic index explained in detail below, offers rough estimates of the food’s predicted glucose impact, monitoring can help in more accurately determining. This includes the determination of which foods will help to prevent glucose spikes after meals, maintain glucose levels within a healthy range, and keep fasting glucose at a low-risk range.
4.Helps to stay within Time in Range
Time in Range (TIR) is a metric that measures the time in which the blood glucose is within the target range. This metric was introduced by the American Association of Clinical Endocrinologists (AACE) in 2017 to be used as part of its Standards of Care Guidelines, which are given to physicians and patients.
The AACE defines Time in Range as ‘the percentage of time spent at or above the lower boundary (70 mg/dL or 4 mmol/L) and below or equal to the upper boundary (180 mg/dL or 10 mmol/L) during a specified period. It is an important measurement for tracking glucose using continuous CGM systems.
Glucose levels fluctuate throughout the day, so it’s normal to see a curve with little peaks and valleys. But the gold standard is 100% TIR (which means all 24 hours). Non-diabetics, who are aiming for optimal metabolic health, would try to stay within a range of 70 to 110 mg/dL for as much of the day as possible. Keep in mind, however, that these are just targets, so they aren’t personalized to your specific situation. You should always consult a medical professional about the right TIR goals for you, which can shift for a variety of reasons, including if you’re pregnant, older, or at high risk of complications.
5.Exercise and Blood Glucose Monitoring
Physical exercise can improve the body’s ability to maintain stable, healthy glucose levels. The positive effects of exercise on metabolic fitness include an increase in glucose transporters travelling to cells (GLUT4 channels), allowing more glucose to enter and lower circulating glucose, as well as greater metabolic flexibility (the ability to switch between different ‘fuel’ sources—glucose and fat).
Real-time, personalized feedback on glucose levels can serve as motivation for people to work out more often as well as provide better insights into the best intensity and timing for an exercise routine.

For athletes, monitoring glucose levels on an ongoing basis can allow them to better control metabolism and fuelling in order to improve athletic performance. CGM sheds light on how the body uses energy before, during, and after an athletic event, and this, in turn, can help to plan for the optimum time to eat, as well as exercise, to ensure peak performance.
How to maintain blood glucose levels in four ways
You can keep your blood glucose levels at an optimum range in a number of ways. A good first step is becoming aware of where your levels stand. Glucose monitoring can provide you with great insights such as glucose variability. Keeping your blood glucose variability under 12% is considered ideal. There are various factors that can help us to maintain blood glucose levels within a low variability range, including the following:
1.Sleep helps in Maintaining Your Blood Glucose Levels
Sleep and glucose metabolism go hand in hand. A lack of sleep can affect glucose regulation by increasing circulating cortisol (a stress hormone), leading to gluconeogenesis (the production of glucose from non-carbohydrate sources).
In a study, it was discovered that 6 days of sleep restriction was associated with an increase in evening cortisol levels and night-time growth hormone concentrations, resulting in a rapid drop in muscle glucose uptake. Due to spikes in blood glucose levels, both of these factors can also reduce insulin sensitivity. In addition, sleep duration affects hormones associated with appetite, including leptin (which soothes hunger) and ghrelin (which stimulates it).
Sleep deprivation offsets the difference between the two hormones, potentially causing metabolic irregularities that can lead to changes in food intake and cause problems like diabetes and metabolic syndrome.

2.Stress
The sympathetic nervous system controls the body’s response to danger – real and perceived. Stress stimulates the sympathetic nervous system, which releases cortisol. Besides regulating blood pressure and blood sugar levels, cortisol is the body’s natural alarm system. As a result of increased glucose levels as an immediate energy source, cortisol inhibits insulin sensitivity in stressful situations. Chronic stress and chronically elevated glucose levels cause the pancreas (which produces insulin to lower glucose levels in the blood) to become less effective at responding to a high glucose stimulus.
3.Exercise helps in Maintaining Your Blood Glucose Levels
Exercise can help us to maintain our glucose levels and also our metabolic flexibility, the ability to use both fat and glucose as energy sources, depending on what type of workout is being performed. High-intensity anaerobic workouts like high-intensity interval training (HIIT), resistance training, or low/moderate-intensity exercises use different fuel sources and thus can have varying effects on our glucose levels.
In most people, the switch in energy use from glucose to fats happens when endurance exercise is moderate or about 60% of maximum oxygen capacity (VO2 max). However, in high-intensity anaerobic activities, which usually tend to be above 80% VO2 max, glucose usually becomes the predominant fuel source. While HIIT enhances cardiometabolic metrics and bone formation, aerobic exercise is associated with fat metabolism.

4.Diet/ Nutrition for Blood Glucose Levels
Glycemic Index (GI) refers to a relative measure of the incremental glucose response per gram of carbohydrate. Consuming low GI foods are known to keep the blood sugar levels low or reduce them. GI measures how the body absorbs or digests foods, affecting the rate at which blood glucose levels rise. Low GI foods are associated with smaller fluctuations in blood glucose levels as compared to foods with high GI.
However, the GI tells only part of the story with regard to the carbohydrate content of food. Some criticize its ranking system for not reflecting a food’s overall healthfulness. In this discussion, both glycemic load and glycemic variability are relevant. Considering a food’s nutritional value as a whole is recommended. The GI ranks carbohydrates in food on a scale from 0 to 100, according to their blood-sugar-raising potential. Although the GI isn’t an exact measurement, it does indicate how the body digests or absorbs food (especially carbohydrates), influencing blood glucose levels.
According to Medicine.net, foods with low (up to 55) to moderate GI (56–69) include legumes, barley, yogurt, oats, and beans. According to a study, a low-carbohydrate diet, high in saturated fat, improved insulin-resistant dyslipoproteinemia without having adverse effects on low-density lipoprotein (LDL, or ‘bad’) cholesterol.
It is also important to avoid high levels of sugary foods and drinks, trans fats, and simple carbohydrates or foods with a high GI and glycemic load. The Mediterranean diet may also reduce insulin resistance. In this diet, the main focus is on eating seasonal foods and using plant-based fats, such as olive oil for cooking and certain fruits for desserts.
Conclusion
The level of glucose in our blood can be an important indicator of our metabolic health. The way glucose is processed and our resultant insulin levels have major implications in terms of the risk of conditions like diabetes, heart disease, and many other chronic conditions. Monitoring glucose levels consistently can help in managing our glucose levels and keeping them within the optimal range between 70 to 110 mg/dL for non-diabetics.
Low glucose variability is generally associated with better health outcomes, and glucose monitoring can help to optimize your weight management, diet, workout routine, and athletic performance. Metabolism is not a one-size-fits-all approach. Tracking our glucose levels can help us understand what makes our blood sugar levels soar and dip and may even suggest optimal times to eat and work out.
Additionally, keeping an eye on one’s sleep, stress, diet, and exercise can help with understanding ways to improve your lifestyle and avoid glucose spikes.
Disclaimer: The contents of this article are for general information and educational purposes only. It neither provides any medical advice nor intends to substitute professional medical opinion on the treatment, diagnosis, prevention or alleviation of any disease, disorder or disability. Always consult with your doctor or qualified healthcare professional about your health condition and/or concerns and before undertaking a new healthcare regimen including making any dietary or lifestyle changes.
References
- Medical Definition of Blood glucose
- Blood Glucose (Blood Sugar): How It’s Made, How It’s Used, Healthy Levels
- Continuous Glucose Monitoring Profiles in Healthy Nondiabetic Participants: A Multicenter Prospective Study | The Journal of Clinical Endocrinology & Metabolism
- Continuous Glucose Monitoring | NIDDK
- Blood Glucose Monitoring: How It WorksGlucose Metabolism – an overview | ScienceDirect Topics