We often visit our doctors for check-ups and get lab tests done, where they look at some of our innate measurable parameters that provide key insights into the state of our health. These criteria are called biomarkers.

Highlights
- Health professionals can make informed decisions regarding the health of their patients by analysing their individual biomarkers,
- Metabolism is the process by which your body converts what you eat and drink into energy,
- Keeping a check on our individual biomarkers is essential to optimise our metabolic health.
What are Biomarkers?
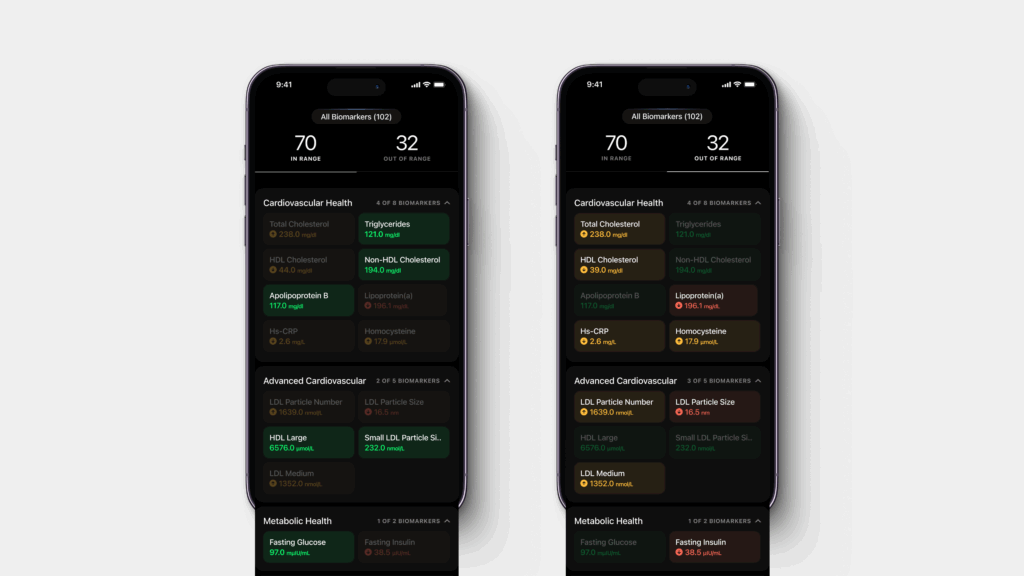
Health professionals can make informed decisions regarding the health of their patients by analysing their individual biomarkers to identify the prevalence of or susceptibility to any particular disease, their causes, and its effects. It is crucial for individuals to track their biomarkers to ensure the maintenance of an optimal lifestyle.
What is Metabolic Health?
Metabolism is the process by which your body converts what you eat and drink into energy. In a study published in the Metabolic Syndrome and Related Disorders, metabolic health is described as having ideal levels of blood sugar, triglycerides, high-density lipoprotein (HDL) cholesterol, blood pressure, and waist circumference, without using medications.
Biomarkers that help measure Metabolic Health
Blood Glucose: Your body breaks down carbohydrates into glucose. Glucose is a form of sugar you get from the foods you eat, and your body uses it for energy. As the glucose travels through your bloodstream to your cells, it is called blood glucose. When blood glucose levels are high, they cause various types of disruptions in the body. High levels mean that your body isn’t making enough insulin, an anabolic hormone that is in charge of regulating blood glucose and helping it enter cells for energy, or isn’t effectively using it. A blood sugar level less than 140 mg/dL (7.8 mmol/L) is considered normal.
Glycemic Index (GI) measures how the body absorbs or digests foods, affecting the rate at which blood glucose levels rise. Consuming low glycemic index foods keeps blood sugar levels low or helps reduce them. Studies show that foods that are low GI (up to 55) to moderate GI (56-69) include legumes, barley, yoghurt, oats, beans, etc.

Insulin Sensitivity: Insulin sensitivity refers to how effectively and efficiently cells respond to insulin. Insulin sensitivity is crucial for our body’s ability to use glucose for energy, to perform bodily functions and store glucose as glycogen in our muscles and liver for future use. Insulin is a hormone created by the pancreas that controls the amount of glucose in a person’s bloodstream at any given moment. It helps store glucose in the liver, fat, and muscles, and regulates the body’s metabolism of carbohydrates, fats, and proteins. After eating, blood sugar levels rise. Insulin released by the pancreas helps the cells to absorb blood sugar for energy and storage. With this absorption, glucose levels in the bloodstream begin to decline. The pancreas then produces glucagon, a hormone that prompts the liver to release stored sugar.
This interaction of glucagon and blood sugar ensures stable blood glucose levels in the body and the brain. The cells of individuals who have insulin resistance don’t respond well to insulin, barring glucose from entering them with ease. The glucose level in their blood rises over time even as their body produces more insulin as the cells resolutely resist insulin. Insulin resistance and insulin sensitivity are inversely related. Having insulin resistance translates into having low insulin sensitivity. While insulin resistance is considered detrimental to your well-being, insulin sensitivity is beneficial to it.
There is no single test that can directly diagnose insulin resistance. Instead, your healthcare practitioner will consider multiple factors, including medical history and symptoms amongst others. There are various tests that can provide varying levels of results based on fasting for 30 minutes, 1 hour and 2 hours after glucose administration.

Heart Rate Variability
A normal resting heart rate in adults ranges from 60 to 100 beats per minute. A lower heart rate at rest implies more efficient heart function and better cardiovascular fitness, as the heart has to spend less energy on heart function. For example, a high-level athlete might have a normal resting heart rate closer to 40 beats per minute.
Heart rate variability is the variance in time between the beats of your heart. So, if your heart rate is 60 beats per minute, it’s not actually beating once every second. Within that minute there maybe 0.9 seconds between two beats, for example, and 1.15 seconds between two others. The greater this variability is, the more “ready” your body is to execute at a high level.
Stress response
Stress impacts metabolic health as stress response starts in the brain. In case of stress or perceived stress, the amygdala (area of the brain that contributes to emotional processing) decodes the sights and sounds and sends an SOS signal to the hypothalamus. The amygdala interprets images and sounds. When it perceives danger, it instantly sends a distress signal to the hypothalamus. The hypothalamus communicates with the body through the autonomic nervous system.
When you experience stress or sense danger (whether real or perceived), the sympathetic nervous system is mobilized. It stimulates the adrenal glands to set off the secretion of catecholamines –including adrenaline and noradrenaline. This leads to a spike in heart rate, blood pressure, and breathing rate. Blood is pushed to the vital organs. These are evolutionary adaptations to increase the chance of survival in life-threatening situations.
Sleep
Sleep is one of the three fundamental pillars of metabolic health, along with exercise and nutrition, each equally important and interdependent on the other. The less you sleep, the shorter your lifespan, adding an unfortunate layer of realism to the old maxim “I’ll sleep when I’m dead”.

The ideal amount of sleep is 7 hours or more per night. Sleep reforms the body’s metabolic state by fine-tuning the balance of insulin and circulating glucose, therefore a lack of it can have a damaging impact on our metabolism. It is no coincidence that lack of sleep has been proven to be one of the key contributors to diabetes.
Sleep also plays a vital role in regulating 2 hormones in our body—leptin, the hormone that is involved in the regulation of our appetite and which tells our body when it is full after a meal; and ghrelin, the hunger hormone, which also regulates appetite, but to inform us when it is hungry. A lack of sleep, therefore, disrupts the pattern of regulation of these hormones and may often result in the need to binge on food on sleepless nights due to decreased leptin and increased ghrelin levels.
Triglyceride levels
Triglycerides are a type of fat that occurs in the blood. When you eat, any calories that your body does not use right away get turned into triglycerides. Those lipid triglycerides then get stored in fat cells so they can be used as energy later. They are the end product of digesting and breaking down fats in food.

If you regularly eat more calories than you burn, particularly from high-carbohydrate foods, you may have high triglycerides, which can lead to a whole host of diseases. We need to keep our triglyceride levels in check to avoid the possibility of any of these diseases. A healthy triglyceride level is considered to be below 150 milligrams per decilitre. There are easy, natural ways to reduce these triglyceride levels, such as 30 minutes of daily exercise, limiting our sugar intake, and eating a fibre-rich diet, just to name a few.
LDL Cholesterol levels
Lipoproteins are substances made of protein and fat that carry cholesterol through your bloodstream. One is low-density lipoprotein or LDL. The other is high-density lipoprotein, HDL. LDL cholesterol is considered to be the ‘bad’ cholesterol because it collects in the walls of your blood vessels, raising your chances of health problems. This cholesterol can accumulate in the blood vessel walls and contribute to the formation of plaque which can result in chest pain, heart attack or stroke. Optimal low-density lipoprotein is 50 to 70 mg/dl.

Blood Pressure
Your heart pumps blood and circulates it around your body in order to provide your cells with oxygen. This pumping of blood puts pressure on the walls of your blood vessels, referred to as blood pressure. We often ignore blood pressure levels at a young age; however high blood pressure occurs slowly in your body, especially when plaque begins building up in your arteries, making your heart pump harder to circulate blood, eventually leading to risks of a stroke or heart disease.
Blood pressure measurement is an essential part of diagnosing and managing hypertension and can be done through small, wearable monitoring devices to monitor your blood pressure. A blood pressure of less than 120/80 mm Hg is considered to be within the normal range. High blood pressure is strongly tethered to obesity. It is often found in people with insulin resistance.
Body temperature
Biomarkers point to either normal or diseased processes in the body. Body temperature is a biomarker for fever. Research suggests that a lower basal body temperature (lowest body temperature attained during rest) may be associated with a prolonged health span. One can use a regular digital thermometer or a basal thermometer. A basal thermometer indicates the temperature in tenths of a degree. It offers insights into tiny changes in body heat.
Body temperature varies throughout the day and also varies by person, age, activity, and time of day. The acceptable normal body temperature is held at 98.6°F (37°C). Some studies have shown that the ‘normal’ body temperature can range from 97°F (36.1°C) to 99°F (37.2°C). A temperature above 100.4°F (38°C) usually means you have a fever caused by an infection or illness.
Respiratory Rate
The respiration rate refers to the number of breaths a person takes per minute. It is usually calculated when a person is at rest and involves counting the number of breaths for one minute by tallying the number of chest rises. It may rise with fever or other medical conditions. Normal respiration rates for an adult person at rest vary between 12 to 16 breaths per minute. According to studies, the clinical measure of respiration, namely Spirometry, is not suitable for continuous use. Pulse oximetry is widely used to monitor oxygen saturation levels.
A low oxygen level in the blood translates into low oxygen in the tissues. In contrast to heart rate variability measures with established stable standards, no such parameters and open tools exist for continuous oxygen saturation time series variability analysis. Respiratory parameters are essential for assessing and predicting risks such as cardiac arrest, sleep apnea, and asthma attack.

Nutritional Biomarkers
Macronutrients
Macronutrients are nutrients that provide calories or energy and are required in appropriate amounts to maintain a healthy lifestyle. Macronutrients can be broadly classified into:
- Carbohydrates: Carbs are made up of sugar, starches and fibre and are the most important source of energy, forming around 45% to 65% of our total energy intake.
- Proteins: Proteins forming around 10%-35% of our total energy intake, are the building blocks of our body and essential for the growth and maintenance of our body tissues and muscles and ensuring efficient functioning of the body.
- Fats: Fats are a source of essential fatty acids that the body cannot make themselves, forming 20%-35% of our total energy intake and essential for efficient hormonal balance and functioning of vital organs, including the heart.
Micronutrients
Micronutrients are nutrients that are required by the body in small amounts for growth and maintenance. Our body does not produce them naturally, and we need to consume them from foods and supplements. There are 2 basic micronutrients:
- Vitamins: Organic substances that are generally classified as either fat-soluble or water-soluble, such as Vitamin E, Vitamin D, Vitamin K, Vitamin C, and B-complex vitamins such as vitamin B6, vitamin B12, and folate.
- Minerals: Inorganic elements present in soil and water which are absorbed by plants or consumed by animals. Major minerals include calcium, sodium, and potassium. Trace minerals include copper, iodine, and zinc which are needed in small amounts.
How to optimise Metabolic Health using Biomarkers?
Putting all the pieces together, it is crucial to track the biomarkers mentioned regardless of how healthy we think we may be and nip any problems in the bud by being consistent with the following activities:
1. Exercise: Regular exercise improves our metabolic health. A balance of the various forms of exercise, like resistance training, cardio, yoga, etc. would be the optimal way of enhancing our metabolic health. However, it is important to pick the exercises that one can sustain over a long period of time.
2. Nutrition: An optimal mix of macro and micronutrients enhances our metabolic health. High protein diets without sufficient fats and carbohydrates can be detrimental. Similarly, a high carb, low protein, low-fat diet can also be detrimental. A study conducted on healthy overweight individuals found that different foods can alter different metabolic reactions, so having the right balance of these foods enhances metabolic health.
3. Sleep: Apart from having a regular sleeping pattern of 7-8 hours, the quality of sleep is essential. A study of adult men monitored for 8 years showed that those subjects who reported interrupted sleep and difficulty maintaining sleep manifested 2-3 times the risk of developing type 2 diabetes. A simple method of enhancing sleep quality is avoiding exposure to our screens closer to bedtime, as blue light inhibits the production of melatonin, the hormone that induces sleep.
Conclusion
Keeping a check on our individual biomarkers and incorporating exercise, nutritious foods, and sleep into our lifestyle is essential to optimise our metabolic health and to ensure that we are not playing catch-up when the markers of metabolic syndrome come knocking at our front door.
Disclaimer: The contents of this article are for general information and educational purposes only. It neither provides any medical advice nor intends to substitute professional medical opinion on the treatment, diagnosis, prevention or alleviation of any disease, disorder or disability. Always consult with your doctor or qualified healthcare professional about your health condition and/or concerns and before undertaking a new health care regimen including making any dietary or lifestyle changes.
References
- High sensitivity of the human circadian melatonin rhythm to resetting by short wavelength light
- Impact of sleep and sleep loss on glucose homeostasis and appetite regulation – PMC
- How to Boost Your Metabolism With Exercise
- Vital Signs (Body Temperature, Pulse Rate, Respiration Rate, Blood Pressure) | Johns Hopkins Medicine
- Basal body temperature as a biomarker of healthy aging – PMC