Polycystic Ovary Syndrome (also known as PCOS) is a severely underdiagnosed and misdiagnosed condition. Since its emotional and psychological aspects are not visible to the naked eye, they are often overlooked. Depression and anxiety are commonly seen in women with PCOS. Research shows that those with the condition are three times more likely to suffer from these disorders.
A systematic review highlights that women with PCOS might be at an increased risk of suffering from depression, anxiety, OCD, and bipolar disorder. The review also found that the severity of symptoms associated with these disorders is higher in women with PCOS than in women without PCOS. Even though the exact cause for the high prevalence is still unknown to science, screening for psychiatric and mood disorders would facilitate early diagnosis, intervention, and treatment for the women in question.
Additionally, a large percentage of those with PCOS have hirsutism—a symptom that drastically impacts a person’s self-confidence. It is associated with feelings of anxiety, depression, and social avoidance partly because of the psychological difficulties associated with it.
As a consequence of symptoms such as hirsutism, abdominal weight gain, and hair thinning, women feel like they don’t have control over their bodies and, in turn, suffer from poor self-esteem and body image issues.

Highlights
- Women with PCOS are three times more prone to suffering from depression and anxiety, but the symptoms are often ignored and overlooked. Screening for mental health disorders among women with this condition needs to be highly encouraged,
- Even though the associations are still being researched, recent evidence posits that poor blood sugar management might be a causative factor for psychiatric and mood disorders,
- A CGM device can be an invaluable resource in assisting people to manage blood sugar levels and reduce the risk of mental health disorders.
How is mental health associated with glycemic control?
Our brain is an organ that has a high energy demand. About half of the energy in the body is used by the brain as fuel to carry out various processes and functions. This means that the brain uses glucose as a primary source of energy. Simply put, blood sugar dysregulation directly affects brain functions.
The existing research highlights a few associations between depression and blood sugar management, such as brain insulin resistance, high glucose levels causing a decrease in the growth of brain cells, high insulin stimulating the production of stress hormones, and the effect of insulin on inflammation and cytokine production.
Besides this, there is an increase in emerging evidence that places emphasis on the link between mood swings and glycemic control. Poor blood sugar management has been associated with a high risk of restlessness, irritability, and mood disruptions, apart from anxiety and depression.
An observational study conducted among a large, diverse group of postmenopausal women found that high glycemic index diets could be a cause of depression in the latter.
Consuming refined grains, sugar-laden beverages, and junk foods were associated with an increased risk of depression. On the contrary, the consumption of fruits and vegetables, dietary fibre, and whole grains was linked with a decreased risk.
In a randomized controlled trial, similar results were seen. In the trial, the effects of a high glycemic load diet and a low glycemic load diet on mood changes and cognitive performance were compared, and it was observed that the former saw worsened mood outcomes as compared to the latter.

Is insulin resistance the culprit?
Insulin resistance is a condition wherein the body becomes ‘resistant’ to insulin due to excessive or chronic exposure to high blood sugar levels. As a result, the body has to produce more insulin to keep up.
In the South Asian demographic, in particular, there is a high prevalence of insulin resistance. In fact, India is known as the diabetic capital of the world.
This means that most people are predisposed to prediabetes and Type 2 diabetes. Given the current scenario, it becomes extremely important and crucial to balance blood sugar levels and reduce glucose spikes in order to limit the risk of suffering from mental health issues. Keeping in mind the numerous links between insulin resistance and mood swings, it can be beneficial to keep an eye on your blood sugar levels to ensure that you have strong mental and emotional health.
Research suggests that about 65-70% of women with PCOS suffer from insulin resistance. 70-80% of these fall in the obese category. This raises the alarm for these women and emphasizes that they might be at a greater risk of suffering from mental health disorders.
In a study conducted on mice, insulin resistance in the brain impacted dopamine turnover and induced anxiety and depression-like behaviours. This suggests that insulin resistance can have a negative impact on the brain and moods.
Dopamine is a ‘happy’ hormone or a neurotransmitter that gives us an intense feeling of pleasure. A new study suggested that increasing dopamine activity could potentially help in the proper absorption and regulation of glucose.
Insulin resistance can impair signalling pathways in the brain and stimulate the production of stress hormones, leading to an abnormal response to stress or the inability to deal with stress. These stress responses, in turn, lead to depressive symptoms.
Reiterating this point, diabetic individuals are 2-3 times more prone to suffering from depression than non-diabetic individuals. This study emphasises that insulin resistance might be playing a significant role here.
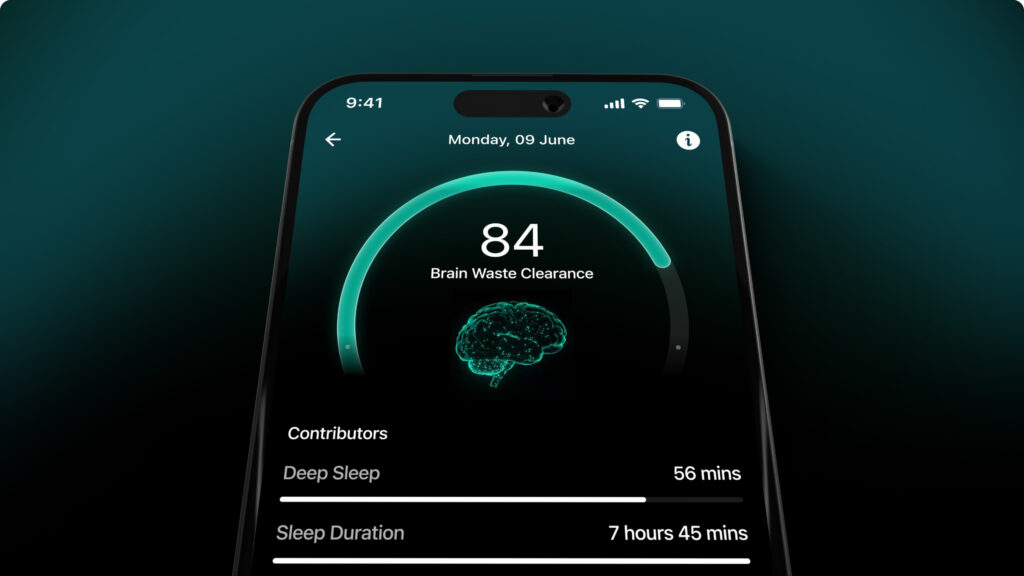
Blood sugar management is vital to managing and dealing with mood and psychiatric disorders. A continuous glucose monitoring (CGM) device can be used as an effective tool to understand how your glucose metabolism works and how different foods affect your blood sugar levels and moods.
Conclusion
With the unfolding of literature and recent evidence that has come to light, the relationship between mental health and glycemic control continues to get stronger.
For those with PCOS, blood sugar management can play a vital role in reducing the risk of suffering from mental health disorders.
Dietary and lifestyle changes directly impact glucose levels and modifications, and improvements to these can lead to a better quality of life and prevent psychiatric and mood disorders. A CGM device can lead to improved glycemic control by giving real-time blood sugar readings and allowing individuals to identify and treat both extreme levels of hypoglycemia and hyperglycemia.
Disclaimer:The contents of this article are for general information and educational purposes only. It neither provides any medical advice nor intends to substitute professional medical opinion on the treatment, diagnosis, prevention or alleviation of any disease, disorder or disability. Always consult with your doctor or qualified healthcare professional about your health condition and/or concerns and before undertaking a new health care regimen including making any dietary or lifestyle changes.
References
- Psychiatric disorders in women with polycystic ovary syndrome: a systematic review and meta-analysis
- Sugar and the Brain
- Is Your Mood Disorder a Symptom of Unstable Blood Sugar?
- High glycemic index diet as a risk factor for depression: analyses from the Women’s Health Initiative
- Long-term effects of provided low and high glycemic load low energy diets on mood and cognition