According to WHO, overweight and obesity are defined as abnormal or excessive fat accumulation that presents a risk to health. A body mass index (BMI) over 25 is considered overweight, and over 30 is regarded obese. The issue has grown to epidemic proportions, with over 4 million people dying each year as a result of being overweight or obese in 2017, according to the global burden of disease. Rates of overweight and obesity continue to grow in adults and children. From 1975 to 2016, the prevalence of overweight or obese children and adolescents aged 5–19 years increased more than four-fold from 4% to 18% globally. Body mass index (BMI) is a calculation that takes a person’s weight and height into account to measure body size. In adults, obesity is defined as having a BMI of 30.0 or more, according to the Centers for Disease Control and Prevention (CDC). Obesity is associated with a higher risk for serious diseases, such as type 2 diabetes, heart disease, and cancer.
The metabolic phenotype is widely considered an important predictor of obesity-related diseases. What does it entail and does it really hold ground? This piece explores the concept.
What is metabolic phenotyping?
Metabolic phenotyping involves the comprehensive analysis of biological fluids or tissue samples. This analysis allows biochemical classification of a person’s physiological or pathological states that relate to disease diagnosis or prognosis at the individual level and to disease risk factors at the population level. These approaches are currently being implemented in hospital environments and in regional phenotyping centres worldwide. The ultimate aim of such work is to generate information on patient biology using techniques such as patient stratification to better inform clinicians on factors that will enhance diagnosis or the choice of therapy. There have been many reports of direct applications of metabolic phenotyping in a clinical setting. [3]
Causes of obesity
Eating more calories than you burn in daily activity and exercise — on a long-term basis — can lead to obesity. Over time, these extra calories add up and cause weight gain. But it’s not always just about calories in and calories out, or having a sedentary lifestyle. While those are indeed causes of obesity, some causes you can’t control.
Common specific causes of obesity include:
- genetics, which can affect how your body processes food into energy and how fat is stored,
- ageing, which can lead to less muscle mass and a slower metabolic rate, making it easier to gain weight,
- not sleeping enough, which can lead to hormonal changes that make you feel hungrier and crave certain high-calorie foods,
- pregnancy, as weight gained during pregnancy may be difficult to lose and might eventually lead to obesity.
Certain health conditions can also lead to weight gain, which may lead to obesity. These include:
- polycystic ovary syndrome (PCOS), a condition that causes an imbalance of female reproductive hormones,
- Cushing syndrome, a condition caused by having high cortisol levels (the stress hormone) in your system,
- hypothyroidism (underactive thyroid), a condition in which the thyroid gland doesn’t produce enough of certain important hormones,
- osteoarthritis (OA) and other conditions that cause pain that may lead to reduced activity (1).

Obesity and metabolic health
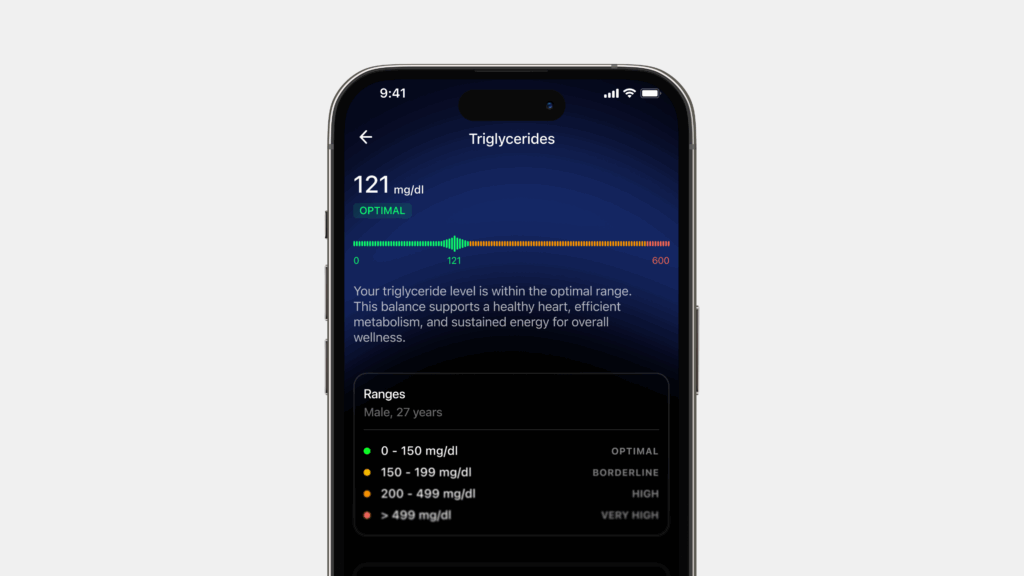
Metabolic health is defined as having ideal levels of blood sugar, triglycerides, high-density lipoprotein (HDL) cholesterol, blood pressure, and waist circumference, without using medications. These factors directly relate to a person’s risk for heart disease, diabetes, and stroke. Obesity is often associated with metabolic abnormalities, including glucose intolerance, type 2 diabetes, dyslipidemia, hypertension, nonalcoholic fatty liver disease, increased inflammation, and metabolic syndrome—all of which increase the risk of cardiovascular diseases (CVD) (ie, coronary heart disease, stroke, and heart failure). [2]
Importance of meta phenotyping in terms of obesity
Obesity phenotypes have been observed in which a subset of obese persons may be considered as having metabolically healthy obesity (MHO) with no evidence of existing cardiometabolic disease. In contrast to MHO, there are also obese persons having metabolically unhealthy obesity (MUO) and an excess risk of adverse cardiometabolic and CVD (Cardiovascular) outcomes. However, the debate continues as to whether individuals with MHO are truly free of adverse CVD outcomes when compared with metabolically healthy nonobese individuals. The evidence has been inconsistent. [4]
Metabolic Phenotyping in Obesity
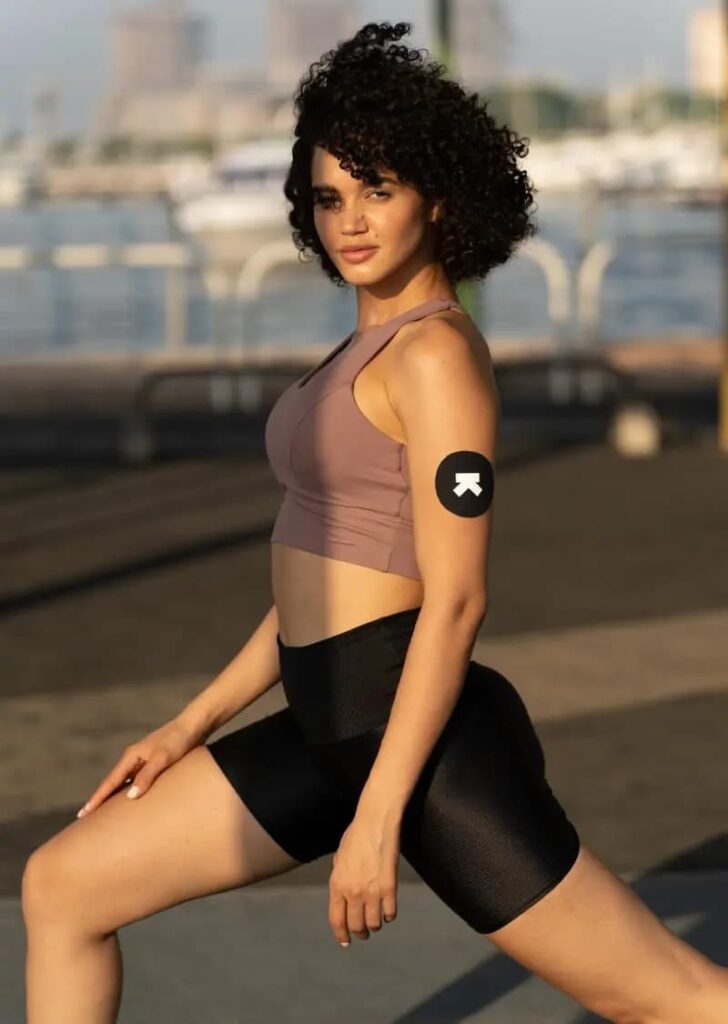
Obesity is a chronic disease that has been linked to insulin resistance and other metabolic dysfunctions. The metabolic phenotype, which includes the set of measurable traits, such as body composition variables and biomarkers related to metabolism, is an important predictor of obesity-related diseases. It has also been observed that different phenotypes appear to have different causes. Some of the phenotypes are:
1. BMI
BMI is a way of measuring the size of an individual’s body. BMI is a measurement for body fat. It is calculated from a person’s weight and height. It is positively associated with risk factors for cardiovascular and metabolic diseases when BMI is above 18.5. BMI does not take into consideration body composition and hence is not an accurate measurement of obesity.
Although total fat mass is a more accurate measure of the metabolic phenotype than BMI, the absolute amount of body fat does not unambiguously reflect metabolic health at an individual level.
The distribution of fat in the body is another way to measure obesity. Fat in different body parts has different correlations to health. Body fat distribution is a strong metabolic and cardiovascular risk factor. Accumulation of adipose tissue in the upper body (abdominal region) is associated with the development of obesity. Adipose tissue is a lipid-storage mechanism that is found in virtually all animals. In contrast, population studies have shown that accumulation of fat in the lower body) is associated with a protective lipid and glucose profile as well as a decrease in cardiovascular and metabolic disease prevalence after adjustment for total body fat mass.
4. Adipose Tissue Function
Adipose tissue can be found in many different parts of the body, but it is most commonly found around the torso (abdomen, lower back, and hips). It has a crucial role in buffering the daily influx of dietary fat entering the circulation. Thus, the ability of our body to adapt to (chronic) changes in caloric intake largely depends on the ability of adipose tissue to accommodate a potential excess of calories. In obesity, the subcutaneous adipose tissue may fail to appropriately expand to store the energy surplus. This in turn may lead to ectopic fat deposition in other tissues involved in metabolic homeostasis (i.e., skeletal muscle, the liver, and visceral adipose tissue). Therefore, the expandability of subcutaneous adipose tissue seems to be a critical factor in health.
What is Metabolically Healthy Obesity?
A person with metabolically healthy obesity has a body mass index (BMI) of over 30, but they do not have metabolic syndrome. Metabolic syndrome consists of high blood pressure, cardiovascular disease, type 2 diabetes, and high cholesterol.
Some studies suggest that up to 35% of people with obesity do not have metabolic syndrome. In other words, they have metabolically healthy obesity. However, some experts believe that this is misleading, as it gives the impression that obesity can be healthy. Other experts believe that the state of metabolically healthy obesity is a passing one. In time, the person will start to develop symptoms of metabolic syndrome. Obesity also increases the risk of other conditions, including respiratory problems and some types of cancer.
There are no guidelines for defining metabolically healthy obesity. There are guidelines to define metabolic syndrome, however. Doctors will diagnose metabolic syndrome if a person has three of the following factors:
- a waist that measures over 40 inches in men or over 35 inches in women,
- fat, or triglyceride, levels in the blood of 150 milligrams per deciliter (mg/dl) or above,
- levels of high density lipoprotein, or “good,” cholesterol below 40 mg/dl in men or below 50 mg/dl in women,
- fasting blood glucose of 100 mg/dl or above,
- blood pressure of 130/85 millimeters of mercury or above.
If a person has obesity but fewer than three of these factors, they are considered to have metabolically healthy obesity. However, if the person does not lose weight, the symptoms of metabolic syndrome may start to appear. Metabolic syndrome can also affect people without obesity, but obesity is a major risk factor. The exact link between obesity and these conditions is unclear, but inflammation appears to play a role. Experts have found that when a person with obesity loses weight, inflammation levels also tend to fall.
Health professionals do not yet know why some people with obesity do not develop metabolic syndrome. Genetic factors may play a role. In 2013, a study found that people with metabolically healthy obesity were more likely to have lower levels of inflammation than those with obesity and metabolic syndrome. A rodent study from 2016 found that some proteins might protect the body from the harmful effects of obesity. More research is necessary to evaluate the effectiveness of these mechanisms in humans, however. Some experts have suggested that the type of fat a person has and where it collects in the body may make a difference. Fat that collects around the lower trunk may be less harmful than fat that accumulates around the abdomen, for example. Another team found that the bodies of metabolically healthy people burn fat more effectively than those of people with metabolic issues such as type 2 diabetes. Research suggests that people with metabolically healthy obesity have a higher risk of developing metabolic abnormalities than people who do not have obesity. However, it is hard to determine if everyone with metabolically healthy obesity will eventually develop metabolic problems. In time, it is possible that everyone with obesity will have metabolic issues if they do not lose weight. Scientists need to conduct more research to determine the risks and causes associated with metabolic syndrome.
Conclusion
Obesity is defined as a disorder involving excessive body fat that increases the risk of health problems. Obesity often results from taking in more calories than are burned by exercise and normal daily activities. It occurs when a person’s body mass index is 30 or greater. Excessive body fat increases the risk of serious health problems. The mainstay of treatment is lifestyle changes such as diet and exercise. Metabolic phenotypes such as fat mass, BMI, body fat distribution & adipose tissue function can be used to determine obesity. While each of them provide great insights into the body, it is important to note that some of them may not give the complete picture. That being said, obesity doesn’t always indicate metabolic syndrome. Many people with obesity develop additional health problems known collectively as metabolic syndrome. However, not everyone with obesity has these complications. Some people call this “metabolically healthy obesity.” While this is an emerging area of interest and research, there are equally strong views for and against it in the medical industry.
Disclaimer: The contents of this article are for general information and educational purposes only. It neither provides any medical advice nor intends to substitute professional medical opinion on the treatment, diagnosis, prevention or alleviation of any disease, disorder or disability. Always consult with your doctor or qualified healthcare professional about your health condition and/or concerns and before undertaking a new health care regimen including making any dietary or lifestyle changes.
References