Serotonin is hailed as the ‘happy hormone.’ It enables communication of our brain cells with other nervous system cells and modulates our mood. It is conducive to our feeling of well-being and also plays a role in regulating metabolic health. Serotonin falls under a category of messengers called neurotransmitters.
Neurotransmitters: Chemical Messengers
Neurotransmitters are often referred to as the body’s chemical messengers. They are the molecules used by the nervous system to transmit messages between neurons, or from neurons to muscles. Communication between two neurons happens in the synaptic cleft (the small gap between the synapses of neurons). Here, electrical signals that have travelled along the axon are briefly converted into chemical ones through the release of neurotransmitters, causing a specific response in the receiving neuron.
A neurotransmitter influences a neuron in one of three ways: excitatory, inhibitory or modulatory. An excitatory transmitter promotes the generation of an electrical signal called an action potential in the receiving neuron, while an inhibitory transmitter prevents it. Whether a neurotransmitter is excitatory or inhibitory depends on the receptor it binds to. Neuromodulators are a bit different, as they are not restricted to the synaptic cleft between two neurons, and so can affect large numbers of neurons at once. Neuromodulators therefore regulate populations of neurons, while also operating over a slower time course than excitatory and inhibitory transmitters.
Most neurotransmitters are either small amine molecules, amino acids, or neuropeptides. There are about a dozen known small-molecule neurotransmitters and more than 100 different neuropeptides, and neuroscientists are still discovering more about these chemical messengers. These chemicals and their interactions are involved in countless functions of the nervous system as well as controlling bodily functions (1)
What functions does Serotonin play in the body?
Serotonin is a monoamine neurotransmitter. Other monoamine neurotransmitters include the catecholamines dopamine, adrenaline, and noradrenaline. These compounds perform several roles including regulation of psychomotor function, cardiovascular, respiratory and gastrointestinal control, sleep mechanisms, hormone secretion, body temperature, and pain. Serotonin is involved in functions such as sleep, memory, appetite, mood, digestion and others. It is also produced in the gastrointestinal tract in response to food. Serotonin is found mostly in the digestive system, although it’s also in blood platelets and throughout the central nervous system. Serotonin is made from the essential amino acid tryptophan. This amino acid must enter your body through your diet and is commonly found in foods such as nuts, cheese, and red meat. Tryptophan deficiency can lead to lower serotonin levels. This can result in mood disorders and also impacts blood glucose levels, such as anxiety or depression.
Our bodies generate serotonin to help your brain cells and other nervous system cells communicate with each other. Serotonin impacts every part of your body, from your emotions to your motor skills. Serotonin is considered a natural mood stabilizer and ushers a feeling of well-being.
Here’s how serotonin acts in various functions across your body
1.Bowel movements: Serotonin is found primarily in the body’s stomach and intestines. It helps control your bowel movements and function.
2.Mood: Serotonin in the brain is found to regulate anxiety, happiness, and mood. Low levels of the chemical have been associated with depression, and increased serotonin levels brought on by medication are thought to decrease arousal.
3.Nausea: The chemical also stimulates the part of the brain that controls nausea.Production of serotonin rises to push out noxious or upsetting food more quickly in diarrhea. Sleep: This chemical is responsible for stimulating the parts of the brain that control sleep and waking. Whether you sleep or wake depends on what area is stimulated and which serotonin receptor is used. Serotonin also plays an important role in the production of melatonin (the sleep hormone). Within the pineal gland, serotonin is acetylated and then methylated to produce melatonin which is an important regulator for normal sleep patterns.
4.Blood clotting: Blood platelets release serotonin to help heal wounds. The serotonin causes tiny arteries to narrow, helping form blood clots. Serotonin contributes to the formation of blood clots. It is released by platelets (disc shaped red blood cells) when there is a wound. The resulting vasoconstriction, or narrowing of the blood vessels, reduces blood flow and helps blood clots to form. When activated, the platelets release the contents of small packages that they carry called delta granules. These packages contain calcium, various energy-containing molecules, and serotonin. When the delta granules are released by activated platelets, the serotonin and other molecules work in the injured area to amplify the coagulation response.
5.Bone health: Serotonin plays a role in bone health. Significantly high levels of serotonin in the bones can lead to osteoporosis, which makes the bones weaker.
6.Sexual function: Low levels of serotonin are associated with increased libido, while increased serotonin levels are associated with reduced libido.
Research connects serotonin with food intake, energy expenditure, hormone balance and nutrient metabolism. Increasing concerns over the health crisis of obesity and diabetes have led to a renewed interest in serotonin pathways in the treatment of metabolic disease.
Metabolism of serotonin is carried out primarily by the outer mitochondrial membrane enzyme monoamine oxidase (MAO), which occurs as two molecular subtypes called MAO-A and MAO-B.
What is serotonin’s role in regulating metabolic health
Serotonin and insulin
Serotonin produced within the central nervous system regulates behavior, suppresses appetite, and promotes energy expenditure by increasing sympathetic drive to brown adipose tissue. In addition to these central circuits, emerging evidence also suggests an important role for peripheral serotonin as a factor that enhances nutrient absorption and storage. Specifically, glucose and fatty acids stimulate the release of serotonin from the duodenum, promoting gut peristalsis and nutrient absorption. Serotonin also enters the bloodstream and interacts with multiple organs, priming the body for energy storage by promoting insulin secretion and de novo lipogenesis in the liver and white adipose tissue, while reducing lipolysis (the breakdown of fats and other lipids by hydrolysis to release fatty acids) and the metabolic activity of brown and beige adipose tissue. Collectively, peripheral serotonin acts as an endocrine factor to promote the efficient storage of energy by upregulating lipid anabolism. Pharmacological inhibition of serotonin synthesis or signaling in key metabolic tissues are potential drug targets for obesity, type 2 diabetes, and nonalcoholic fatty liver disease (NAFLD).
Serotonin and weight loss
More than 30 years ago, extensive studies at MIT carried out by Richard Wurtman, M.D., showed that tryptophan, the building block of serotonin, could get into the brain only after sweet or starchy carbohydrates were eaten. Although tryptophan is an amino acid and found in all proteins, eating protein prevents tryptophan from passing through a barrier from the blood into the brain. The reason is simply numbers: Tryptophan competes for an entry point into the brain with some other amino acids. There are more of those other amino acids in the blood than tryptophan after protein is eaten. So in the competition to get into the brain, tryptophan is at a total disadvantage and very little gets in after a protein meal like turkey or snack like yogurt.
But carbohydrates tip the odds in tryptophan’s favor. All carbohydrates (except fruit) are digested to glucose in the intestinal tract. When glucose enters the bloodstream, insulin is released and pushes nutrients such as amino acids into the cells of the heart, liver and other organs. As it does this, tryptophan stays behind in the bloodstream. Now there is more tryptophan in the blood than the competing amino acids. As the blood passes by the barrier into the brain, tryptophan can get in. The tryptophan is immediately converted to serotonin, and the soothing and appetite controlling effects of this brain chemical are soon felt.(2)
Over the past several decades, multiple studies have established the role of serotonin in reducing food intake and promoting satiety. For instance, inhibition of serotonin is orexigenic. This simply means that serotonin restriction could lead to an increase in appetite and hunger, which can enhance food consumption and in extreme cases it may lead to obesity.(5)
Research corroborates that both gut-derived circulating serotonin and adipocyte-derived serotonin are instrumental in adipose tissue function. [9]
According to a study conducted, a leading psychology publication volunteers found that when people consumed a pre-meal carbohydrate drink that made more serotonin, they became less hungry and were able to control their calorie intake. Volunteers whose drinks contained protein—so that serotonin was not made—did not experience any decrease in their appetite. A counter study to this says that potential beneficial outcomes associated with protein ingestion include the following: 1) increased satiety—protein generally increases satiety to a greater extent than carbohydrate or fat and may facilitate a reduction in energy consumption under ad libitum dietary conditions; 2) increased thermogenesis—higher-protein diets are associated with increased thermogenesis, which also influences satiety and augments energy expenditure.
Most of us have experienced the carbohydrate-serotonin effect on our appetite even though we were not aware of the connection. Have you ever munched on rolls or bread while waiting for the main course to be served in a restaurant? By the time dinner is served, twenty minutes or so after you ate the roll, your appetite has been downsized. “I don’t even feel that hungry” is a common response when the plate is put down on the table.
This blunting of appetite is not because you may have eaten 120 calories of roll. It is caused by new serotonin putting a brake on your appetite.(3)

Serotonin and heart health
“A less active brain serotonin system is associated with early hardening of the arteries, according to a study presented by University of Pittsburgh researchers at the 64th Annual Scientific Conference of the American Psychosomatic Society in Denver. These findings, which are the first to establish a link between serotonin messages in the brain and atherosclerosis, could lead to an entirely new strategy for preventing heart disease and stroke, say the researchers. Many of the known risk factors for heart disease and stroke — high blood pressure and cholesterol, obesity, diabetes, smoking and lack of exercise — can, to some extent, be controlled by our lifestyle choices” said Matthew F. Muldoon, M.D., M.P.H., associate professor of medicine, University of Pittsburgh School of Medicine. “Until now, no one had studied the possibility that brain abnormalities could explain why some people make these poor lifestyle choices and have multiple risk factors for heart disease.”
Serotonin & gastrointestinal function
Serotonin regulates gastrointestinal function. The gut is surrounded by enterochromaffin cells, which release serotonin in response to food in the lumen. This makes the gut contract around the food. Platelets in the veins draining the gut collect excess serotonin. There are often serotonin abnormalities in gastrointestinal disorders such as constipation and irritable bowel syndrome. [6]
If irritants are present in the food, the enterochromaffin cells release more serotonin to make the gut move faster, i.e., to cause diarrhea, so the gut is emptied of the noxious substance. If serotonin is released in the blood faster than the platelets can absorb it, the level of free serotonin in the blood is increased. This activates 5-HT3 receptors in the chemoreceptor trigger zone that stimulate vomiting. [6] Thus, drugs and toxins stimulate serotonin release from enterochromaffin cells in the gut wall. The enterochromaffin cells not only react to bad food but are also very sensitive to irradiation and cancer chemotherapy. Drugs that block 5HT3 are very effective in controlling the nausea and vomiting produced by cancer treatment, and are considered the gold standard for this purpose. [7]
Research shows that microbes in the gut help produce serotonin. This production might be disrupted when the microbiome, or gut bacteria as a whole, is disturbed because of stress, disease, diet, or other causes. According to this study, low central serotonergic activity is associated with metabolic syndrome. [8]
Serotonin Imbalance
Serotonin deficiency is a complex condition for which there are no diagnostic criteria and no clear tests. It’s generally discussed in terms of the symptoms that result, rather than the exact levels that might bring it on. Serotonin deficiency has been linked to many physical and psychological symptoms. However, its exact role in any of them isn’t fully understood. Much research continues within the medical and scientific communities. Research has found that the overwhelming amount of serotonin in your body — 95 percent — is produced in the lining of your gastrointestinal (GI) tract. The remaining 5 percent is produced in your brain.
Some research about serotonin has to do with its role in what is called the gut-brain axis. This is a communication line between the central nervous system and the enteric, or intestinal, nervous system. This effectively links the brain and the gut, giving rise to the name: gut-brain axis.
Serotonin deficiency may be a contributing factor in many psychological and physical symptoms.
Psychological symptoms
Serotonin deficiency is associated with many psychological symptoms. These may include:
- anxiety,
- depressed mood,
- aggression,
- impulsive behavior,
- insomnia,
- dementia and cognitive decline.
Low serotonin levels are also associated with various behavioral and emotional conditions, including:
- obsessive-compulsive disorder (OCD),
- panic disorder,
- suicidal behavior,
- post-traumatic stress disorder (PTSD),
- social anxiety disorder.
In the brain, serotonin acts as a neurotransmitter or chemical message which is being sent across the gap called the synapse between nerve cells. The cell sending the message, called the presynaptic cell, releases serotonin into the synapse. The serotonin is taken in by the receiving, post-synaptic cell, or be taken back by the presynaptic cell. In depression the postsynaptic cell doesn’t take in enough serotonin and the message gets lost. [9]
If the brain produces too much serotonin on the other hand, it could lead to excessive nerve cell activity. Excessive serotonin on the other hand can lead to symptoms that can range from mild (shivering and diarrhea) to severe (muscle rigidity, fever and seizures) and cause serotonin syndrome. Untreated severe serotonin syndrome can be lethal. Increasing the dose of certain medications or including a new drug to your regimen can cause this condition. Scientists are unsure what causes serotonin deficiency. Some research shows early life stressors might negatively affect the transport of serotonin in the body. Other research shows that microbes in the gut help produce serotonin. This production might be disrupted when the microbiome, or gut bacteria as a whole, is disturbed because of stress, disease, diet, or other causes. Both of these studies were done with animals, and researchers emphasized that further clinical research is needed.
Chronic stress is known to affect serotonin (5HT) neurotransmission in the brain and to alter body temperature. Chronic stressors have the potential to lower serotonin levels.
Other potential causes of serotonin deficiency include
- nutritional deficiencies,
- digestion issues,
- certain drugs,
- hormone changes,
- lack of sunlight.
Lower levels of serotonin are also thought to be related to a person’s particular biology, which may include
- fewer or less effective serotonin receptors,
- a body that breaks down serotonin or absorbs it too soon,
- low levels of substances used to produce serotonin, including L-tryptophan, vitamin D, vitamin B6, and omega-3 fatty acids.[8]
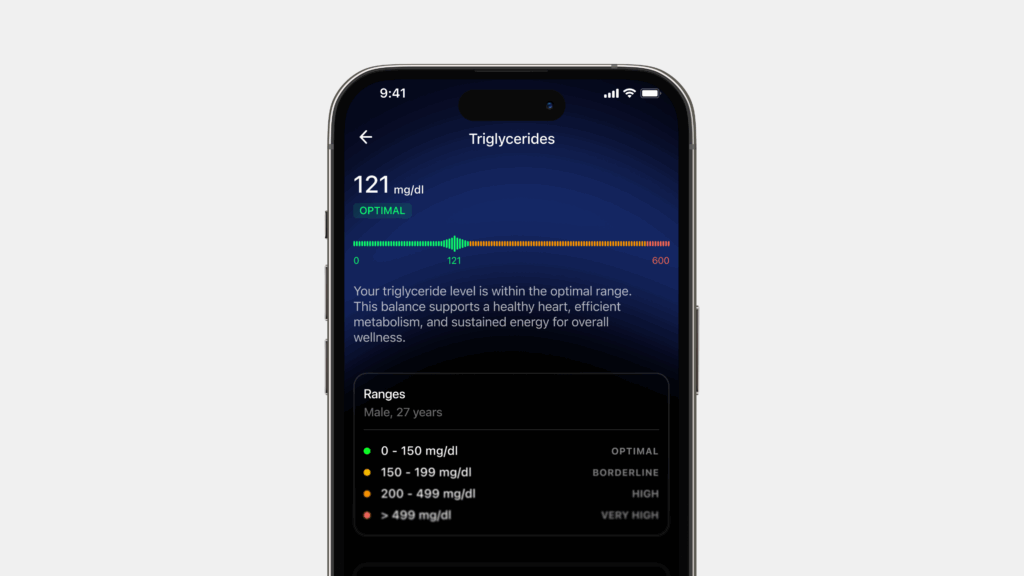
Serotonin levels for optimum health
The typical range for serotonin levels in your blood is considered 101–283 nanograms per milliliter (ng/mL). This standard, however, may vary slightly depending on some testing parameters. It’s prudent to talk to your doctor about specific test results. High levels of serotonin may be a sign of carcinoid syndrome (tumors of the small intestine, appendix and colon).
When serotonin levels are optimal we experience a great mood during the day and a restful sleep at night. When serotonin levels are low so is our self-confidence. This is because serotonin keeps the right and left hemisphere of the brain in balance. When this balance is compromised it would result in a disconnection between the brain’s left side’s rationality and the right side’s creativity and as a consequence lead to low mood, depression and trouble falling asleep.[9]
How to optimise serotonin levels
- Low serotonin levels could mean that the brain is making less serotonin, or has fewer receptors for it, or those receptors just aren’t grabbing on to the serotonin very well. It can also mean the serotonin that’s made is broken down too soon, or that the serotonin that’s released out into the synapse is sucked too quickly back into the presynaptic neuron. Studies show that changing any one of these factors can increase serotonin activity.
- One way to increase serotonin levels is by frequent exposure to sunlight. This is because serotonin production in the brain is directly related to the duration of bright sunlight. Recent research provides more evidence that lack of sunlight and reduced serotonin levels are important in the development of seasonal affective disorder (SAD). People with SAD develop symptoms of depression in the winter months when there is less daylight. Symptoms include difficulty concentrating, low energy or fatigue, loss of interest in daily activities, moodiness, and sleeping excessive amounts.
- The positive effect sunlight has on serotonin levels is because it enables synthesis of Vitamin D. Serotonin synthesis, release, and function in the brain are modulated by vitamin D and the 2 omega-3 fatty acids, eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). Brain serotonin is synthesized from tryptophan by tryptophan hydroxylase 2, which is transcriptionally activated by Vitamin D hormone. Therefore, inadequate levels of Vitamin D and Omega-3 fatty acids would lead to reduced production of serotonin .
- Exercise is equally important to boost serotonin levels. In particular, aerobic exercise, like running and biking, is most likely to boost serotonin. However, yoga works too. In addition, exercise would also increase the levels of the serotonin precursor, tryptophan which is important for the synthesis of serotonin.
- Meditation practices have various health benefits including the possibility of increasing serotonin levels, preserving cognition and preventing dementia. While the mechanisms remain investigational, meditation may affect multiple pathways that could play a role in brain aging and mental health. Researchers have shown that activities like mindfulness have a direct impact on the brain’s production of serotonin levels. It is thought that meditation “bathes” neurons with an array of feel-good chemicals. Meditation also reduces stress‐induced cortisol secretion and this could have neuroprotective effects potentially via elevating levels of brain derived neurotrophic factor (BDNF). Meditation may also potentially have beneficial effects on lipid profiles and lower oxidative stress, both of which could in turn reduce the risk for cerebrovascular disease and age‐related neurodegeneration. Further, meditation may potentially strengthen neuronal circuits and enhance cognitive reserve capacity (Xiong & Doraiswamy, 2009).
Conclusion
Serotonin is a type of neurotransmitter that helps regulate moods and emotions. Serotonin is the brain’s “happy hormone” and it is released when you feel happy or content. It controls the release of other neurotransmitters, such as dopamine, which can lead to feelings of euphoria. Serotonin also helps improve sleep quality by promoting serotonin-melatonin signalling across the brain. When serotonin levels drop, it can cause problems with your mood and even your appetite.
The majority of serotonin is distributed to many parts of the body and only a small amount (around 2%) is present in the central nervous system and brain. This 2% plays a pivotal role in mood-related disorders. Low levels of serotonin is also known to impact sleep and bowel movement. Though the exact mechanism is yet to be fully understood, research suggests that serotonin may serve an essential role in regulating the release of insulin and glucagon, the two main hormones that control glucose and lipid homoeostasis, improving insulin sensitivity and glucose metabolism. Serotonin is nature’s own appetite suppressant. This powerful brain chemical curbs cravings and shuts off appetite and can aid in weight loss. Low central serotonergic activity is associated with metabolic syndrome. Exercise, nutrition, meditation and adequate sunlight is known to beneficially impact serotonin levels.
References
- https://www.healthline.com/health/mental-health/serotonin#takeaway
- https://www.psychologytoday.com/us/blog/the-antidepressant-diet/201008/serotonin-what-it-is-and-why-its-important-weight-loss#:~:text=by%20Jessica%20Schrader-,Serotonin%20is%20nature’s%20own%20appetite%20suppressant.,eating%20less%20and%20losing%20weight.
- https://pubmed.ncbi.nlm.nih.gov/30901029/
- https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-016-0201-1
- https://www.sciencedaily.com/releases/2006/03/060303205220.htm