Some of the innate measurable parameters that provide key insights into different aspects of our health are known as biomarkers. Health professionals can make informed decisions regarding the health of patients by analysing individual biomarkers to identify the prevalence of or susceptibility to a particular disease, and its causes and effects. It is crucial for individuals to track their biomarkers to maintain an optimal lifestyle.
Body temperature is one of the most basic biomarkers linked with various aspects of our health, including metabolic health, sleep, stress and almost every other bodily function. Body temperature has long been recognised as a key indicator of health; it is easy to measure and can vary depending on a number of factors. It can also provide a lot of information about our health.
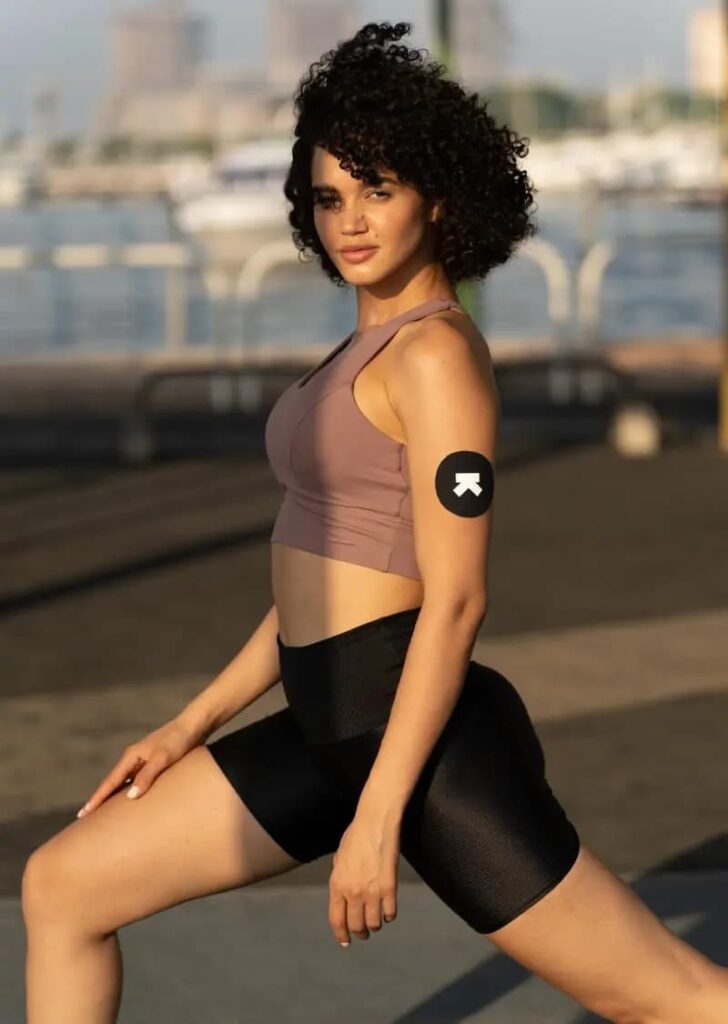
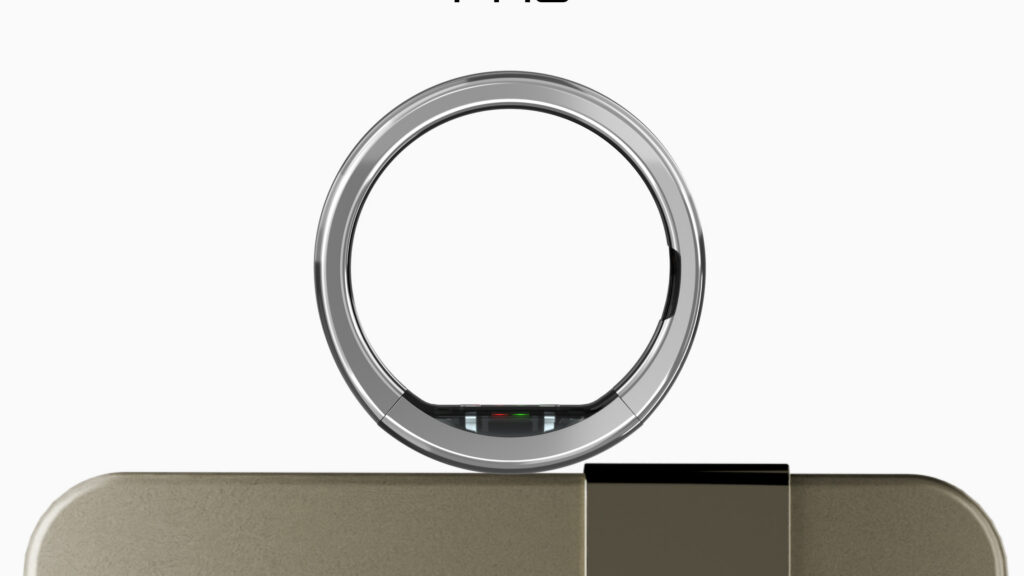
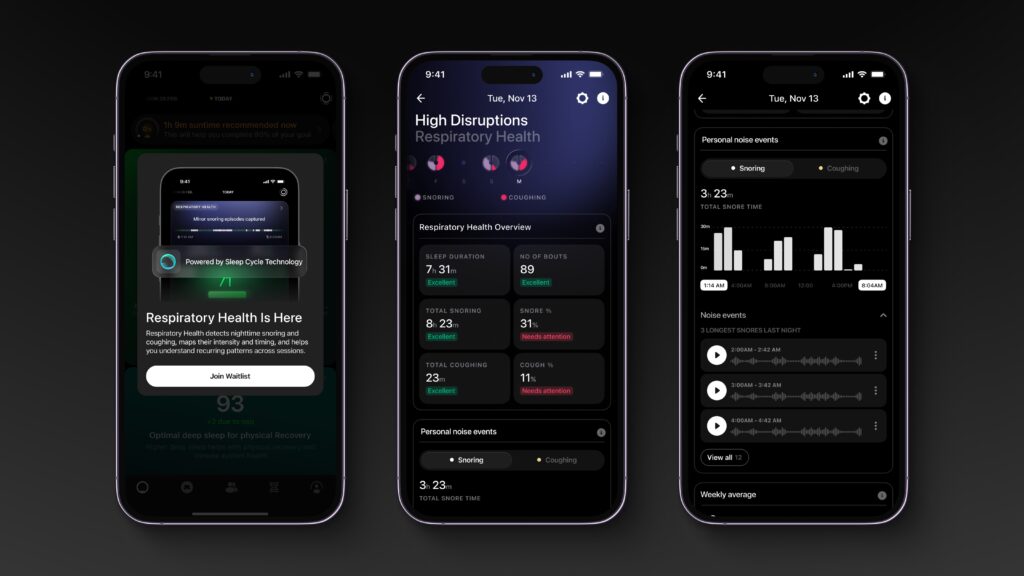
Learn: How Ultrahuman Ring AIR tracks skin temperature
Ideal Body Temperature
Body temperature is a measure of how well an organism is able to generate and get rid of heat. The normal body temperature, which changes throughout the day, varies by person, age, time of day and activity level. The average normal body temperature is 98.6 degrees Fahrenheit (37°C). A few studies have shown that the ‘normal’ body temperature can range from 97 degrees Fahrenheit (36.1°C) to 99 degrees Fahrenheit (37.2°C). Body temperature undergoes significant fluctuation over the course of a day. This is called ‘diurnal variation’. It is usually at its lowest early in the morning and slowly climbs up after a person wakes up, reaching its peak in the late afternoon. This variation corresponds to the level of metabolic activity, which is lowest during sleep and increases as the day progresses.
The human body generates heat capable of raising body temperature by approximately 1°C per hour. Normally, this heat is dissipated by means of a thermoregulatory system. Disorders resulting from abnormally high or low body temperature result in neurologic dysfunction and pose a threat to life.
What is Thermoregulation?
Thermoregulation is a term used to describe how our body maintains the internal/core temperature despite the changes in the external environment. It is defined as the mechanism that allows your body to maintain its core internal temperature. All thermoregulation mechanisms are designed to return your body to homeostasis, or a state of equilibrium. Human beings have a normal core internal temperature of around 98.6 degrees Fahrenheit (37°C). This is the optimal temperature at which all of the human body’s systems function.
Read next: Factors affecting skin temperature explained
Maintaining this temperature within a range of 1–2 degrees is the primary function of thermoregulation, which is crucial for all organs to work properly. Without thermoregulation, the human body would cease to function. Thermoregulation is controlled by the hypothalamus in the brain. When the internal temperature changes, sensors in the central nervous system (CNS) send messages to the hypothalamus. In response, it sends signals to various organs and systems in the body that trigger different mechanisms to raise or reduce body temperature.
For example, if the body is generating heat during exercise or if the external ambient temperature is elevated enough to cause a rise in the core temperature, afferent signals to the hypothalamus result in efferent signals to the cells of the skin to produce sweat. Afferent and efferent neurons refer to various types of neurons that make up the sensory and motor divisions of the peripheral nervous system, respectively. Thermoregulatory responses can be either behavioural—for instance, changes in posture or location with regard to the environment—or autonomic,which means internal processes that lead to vasodilation (the widening of your blood vessels), thermogenesis (dissipation of energy through the production of heat) and so on (like sweating, shivering, etc.)
Thermoregulation is a natural and critical process that occurs throughout the course of every day. The body’s natural temperature regulation processes can be impacted by a number of factors ranging from metabolism to digestion to external temperatures.
What is Metabolism and Metabolic Health?
Metabolism is defined as a series of chemical processes in each cell transforming the calories we eat into fuel to keep us alive. These processes sustain life and everyday functioning. They include breaking down food and drink to energy and building or repairing our bodies. Metabolic rate is the rate at which our body expends energy. Your metabolic rate is influenced by many factors, including age, gender, muscle-to-fat ratio, amount of physical activity and hormone function. Basal metabolic rate (BMR) refers to the amount of energy your body needs while at rest to maintain homeostasis. BMR is the amount of energy the body requires to keep all its systems functioning correctly (such as breathing, keeping the heart beating to circulate blood, growing and repairing cells and adjusting hormone levels). Like body temperature, the metabolic rate is unique to each individual and can vary due to external factors such as age, weight, muscle mass, gender, among others.
Metabolic health, meanwhile, is described as having ideal levels of blood sugar, triglycerides, high-density lipoprotein (HDL) cholesterol, blood pressure and waist circumference, without using medications. These biomarkers are indicative of all components of metabolism functioning properly. Body temperature can serve as a useful indicator of metabolism, metabolic health and other functions that it interacts with.
Body Temperature and Metabolic Rate
Research shows that higher core body temperatures appear to increase metabolism. A review published in 2009 in Transactions of the American Clinical and Climatological Association reports that an increase in body temperature is associated with a higher metabolic rate, and higher body temperatures do speed up metabolism. So, body temperature is a fairly reliable guide to metabolic rate.
When people lose weight, their body temperature drops as their metabolism slows down. This is why some people feel cold all the time when they’re dieting, especially if it’s a crash diet. Various studies have shown that there is a connection between the amount of calories consumed and the body temperature, which is directly tied to metabolism. Keeping track of your body temperature can help you determine what kind of metabolic response your body is having to a particular diet or workout routine.
Body temperature can also serve as a marker of metabolic activity because it is linked to energy expenditure and correlates with muscle mass, thyroid activity and metabolic regulation of compounds like glucose, fats and so on.
Body Temperature and Glucose
Temperature regulation in the body is affected when metabolic function is disrupted and glucose levels are elevated. The heat we produce in our bodies is the result of countless chemical reactions occurring in every cell. This heat production is generally matched with an equal heat dissipation, ensuring body temperature stays in a narrow range. According to a study, within minutes of consuming a meal containing carbohydrate and/or protein, both humans and rodents exhibit an increase in energy expenditure and body temperature, typically described as diet-induced or meal thermogenesis. This is because, after a meal, the digestive system converts food into glucose, which subsequently floods the bloodstream. The process of converting this glucose into energy or storing it as fat leads to a momentary increase in temperature. Recent studies have implicated the hormone leptin and brown adipose tissue (BAT) as key drivers of postmeal thermogenesis.
In people with diabetes or chronically raised glucose levels, thermoregulation is slightly compromised and their body temperatures often tend to be higher. This is because of blood vessels – to effectively remove heat from the body, we need a hemodynamic (Hemodynamics are the dynamics of blood flow) shift that arises from coordinated changes in the size of blood vessels throughout the body—blood vessels in the core of the body constrict, and those at the periphery (i.e. skin) dilate. These changes allow the body to transfer the heat from deep within the body to the skin and eventually to the air around the body. Moreover, insulin, a hormone that is crucial to glucose regulation, has been found to directly impact core body temperature. People who have insulin resistance, thus, face difficulties in thermoregulation.
Body Temperature and Sleep
Thermoregulation plays an important role in enabling sleep, and the mechanisms that make this possible are also tied to the hypothalamus and the nervous system. Thermoregulatory behaviour prior to sleeping is a core part of maintaining energy balance and presents in many ways.
For starters, our bodies make a few changes—such as slowing down metabolism and stimulating other heat loss mechanisms— to lower our core body temperature prior to and during sleep. Studies suggest this slight drop in core temperature is an essential part of falling and staying asleep, as it helps stimulate drowsiness.
Thermoregulation also plays a role in waking us up. As morning arrives, our bodies start to naturally raise our body temperature again. This helps wake us up and makes us more alert once we get out of bed. These natural body temperature fluctuations of cooling before sleep and warming up before waking are intimately linked to our body’s circadian rhythms. When functioning properly, these rhythms follow an approximately 24-hour cycle that helps us sustain a regular sleep-wake schedule.
Body Temperature and Stress
Stress is another factor that impacts the body temperature. In humans (and rats), body temperature rises with stress. Technically, this is called stress-induced hyperthermia. This has mostly been studied in acute stress, but some studies have also found a chronic temperature increase with long-term stress.
This increase in temperature is an adaptive response of the body to deal with perceived threats. Adrenaline, which mediates the body’s ‘fight or flight’ response, stimulates increased heat production in the liver in addition to driving other adaptive changes. The liver, as one of the body’s most metabolically active organs, has a notable impact on body temperature.
Moreover, stress can cause a fever even when there is no underlying illness or infection. This is known as a psychogenic fever. Essentially, stress seems to raise core body temperature in the absence of other inflammatory processes such as infection or injury. This is either because the brain increases temperature in response to stress or stress hormones, like cortisol, interact with the endocrine system and lead to an increase in body temperature. For example, a 2020 study published in the journal Science found that the stress response affects the hypothalamus in rats, which is the part of the brain that controls body temperature. But more research is needed to determine whether the mechanism is the same for humans.
Body Temperature and Metabolic Health
People with good metabolic health have more variation in daily temperature; their highs are higher and their lows are lower. They also have more consistency from day today.
This study found that metabolically healthy people have a spikier circadian temperature rhythm (bigger differences between the low and the high point) than inactive people. The study compared people with no metabolic problems to people with at least one symptom of metabolic syndrome (glucose regulation problems, large waist circumference, low HDL cholesterol, and/or high triglycerides). The healthy group had a typical temperature variation of about 1.5 degrees Celsius, while the unhealthy group varied less than 1 degree Celsius.
In fact, body temperature has been found to be an indicator of various factors related to metabolic health and metabolic disorders, such as obesity, cardiovascular health and glucose regulation, as detailed below.
Body Temperature and Obesity
A new study suggests that a biological inability to create sufficient core body heat could be linked to the obesity epidemic. “Evidence of a diurnal (of or during the day) thermogenic (heat-producing) handicap in obesity” was found in subjects who were obese. Human obesity is associated with increased heat production; however, subcutaneous adipose tissue provides an insulating layer that impedes heat loss. To maintain normal thermoregulation, therefore, obese individuals must increase their heat dissipation. This suggests that people affected by obesity have a reduced ability to expend energy as heat, which could result in long-term weight gain.
The scientific reason behind this is linked to brown fat adipose tissue, which breaks down blood sugar (glucose) and fat molecules to create heat and help maintain body temperature. Brown fat contains many more mitochondria than white fat. Brown adipose tissue (BAT) produces heat by burning triglycerides that are stored within intracellular lipid droplets. A study found that this tissue (brown fat) was interlinked with compounds called branched chain amino acids (BCAAs), which play an important role in energy expenditure. People with low brown fat activity had higher levels of BCAAs, which was linked with obesity, insulin resistance and type 2 diabetes.
Body Temperature and Cardiovascular Health
The way the body breaks down food into energy can trigger changes in body temperature that can serve as indicators of even cardiovascular health. Triglycerides, cholesterol and other essential fatty acids—the scientific term for fats that the body can’t make on its own—store energy, insulate us and protect vital organs. They act as messengers, helping proteins do their jobs. They also start chemical reactions that help control growth, immune function, reproduction and other aspects of basic metabolism.
The cycle of making, breaking, storing and mobilising fats is at the core of how humans and animals regulate their energy. An imbalance in any step can result in disease, including heart disease and diabetes. For instance, having too many triglycerides in the bloodstream raises our risk of clogged arteries, which can lead to heart attack and stroke. A study found that in people with poor metabolic health or conditions, like obesity and diabetes, levels of HDL-cholesterol may affect the postprandial regulation of body temperature.
In extreme cases, the changes in the cardiovascular system that develop in chronic heart failure obviously affect thermoregulation. A constant, normal body temperature is the consequence of a regulated balance between heat production and heat loss. Both sides of this balance are seen to be altered in chronic heart failure. Another study found that patients with cardiovascular or metabolic conditions leading to chronic cardiac incidents tend to have disordered thermoregulation, and that high body temperature can often be a marker of cardiac disease.
Body Temperature and Inflammation
We know that overall health and the ability to fight off infection are often associated with a fever or increased body temperature. However, fevers aren’t just a byproduct of our immune response. In fact, it’s the other way around: an elevated body temperature triggers cellular mechanisms that ensure the immune system takes appropriate action against the offending virus or bacteria.
A study recently published in PNAS reveals that higher body temperatures drive the activity of certain proteins that, in turn, switch genes responsible for the body’s immune response on and off, as required.
Essentially, body temperature can serve as a marker of metabolic health in a number of ways as thermoregulation is intricately tied to the way we expend energy at a cellular level, and hence to a variety of indicators of metabolic health such as levels of blood sugar, triglycerides, HDL cholesterol, blood pressure and waist circumference.
Conclusion
Overall, body temperature can be an indicator for various aspects of health. From metabolic rate to sleep patterns to stress levels, it is tied to all these functions. Moreover, thermoregulation is closely linked to metabolic health in a number of ways, including glucose regulation, obesity, cardiovascular health. Changes in temperature show a link with various metabolic or health disorders.
It is important to measure body temperature consistently and be aware of what changes in it may indicate in terms of metabolic rate, stress levels, circadian rhythm or overall metabolic health/physical fitness.
Disclaimer: The contents of this article are for general information and educational purposes only. It neither provides any medical advice nor intends to substitute professional medical opinion on the treatment, diagnosis, prevention or alleviation of any disease, disorder or disability. Always consult with your doctor or qualified healthcare professional about your health condition and/or concerns and before undertaking a new health care regimen including making any dietary or lifestyle changes.
Resources
- https://pubmed.ncbi.nlm.nih.gov/24365362/
- https://blog.ultrahuman.com/biomarkers-to-track-for-metabolic-health
- https://www.onio.com/article/factors-that-influence-your-body-temperature.html
- https://www.fbscience.com/Landmark/articles/pdf/Landmark1054.pdf
- https://blog.ultrahuman.com/metabolism-breaking-down-the-basics