Maintaining stable blood glucose levels is critical for energy, mood, and long-term metabolic health.
If you’re managing prediabetes, aiming to boost athletic performance, or simply trying to avoid the afternoon slump, understanding how your body responds to food, sleep, stress, and exercise is key.
In this guide, we explore why tracking blood sugar matters, what causes glucose levels to rise or fall, and how to optimize them for better performance and disease prevention.
Highlights
- Glucose provides essential energy for the body’s daily functions.
- Insulin regulates blood glucose by facilitating its storage and use.
- Disrupted glucose metabolism can contribute to metabolic syndrome and chronic diseases.
- Check food items with the Open Glucose Database to understand their potential impact.
What is glucose?
Glucose is a monosaccharide – a simple sugar derived from carbohydrate digestion. It is a primary energy source for cells, alongside fat. Foods such as bread, fruits, vegetables, and dairy contribute to glucose levels. The body tightly regulates glucose through complex feedback loops involving insulin and other hormones.
What is insulin?
Insulin, produced by the pancreas, is essential for maintaining blood glucose balance. It promotes the storage of glucose in the liver, fat, and muscles, and plays a key role in metabolizing carbohydrates, fats, and proteins.
What is insulin resistance?
Insulin resistance occurs when cells fail to respond adequately to insulin. This leads to elevated blood glucose levels and can progress to prediabetes or type 2 diabetes if unaddressed [NIH, 2022].
What is insulin sensitivity?
Insulin sensitivity reflects how effectively your cells respond to insulin. High sensitivity means the body uses glucose efficiently. Lifestyle interventions, like physical activity and dietary changes, can enhance sensitivity.
What is glucose metabolism?
Glucose metabolism starts when carbohydrates are digested into simple sugars: glucose, fructose, and galactose. Fructose (from fruit) and galactose (from dairy) are converted into glucose in the liver. Glucose is then either used immediately or stored as glycogen or fat.
How does the body process glucose?
The glucose moves through the body in the following sequence:
- Carbohydrate ingestion triggers receptors in the gut and pancreas.
- Hormones like GLP-1 stimulate insulin production.
- Enzymes (e.g., amylase, sucrase) break down complex carbs.
- Glucose enters the bloodstream and is transported via GLUT and SGLT channels.
- Insulin helps cells absorb glucose. In muscle/fat tissue, it activates GLUT4 transporters.
- Excess glucose is stored as glycogen or converted to triglycerides.
- When needed, glycogen is broken down (glycogenolysis) or new glucose is created (gluconeogenesis).
What is gluconeogenesis?
Gluconeogenesis is the synthesis of glucose from non-carbohydrate sources like lactate, amino acids, and glycerol. It occurs primarily in the liver and is regulated by cortisol and insulin [PubMed PMID: 30335203].
What is glycogenesis?
Glycogenesis is the conversion of glucose into glycogen, mainly in liver and muscle cells. Insulin promotes this process. When glycogen storage is full, surplus glucose is converted to fat.
What is Glycemic Variability?
Our glucose levels give us an insight into our bodies when they vary over time. A metric known as glycemic variability (glucose variability) can be used to identify these internal oscillations in blood glucose levels, measured by how they vary over time. The SD (Standard Deviation) is the most widely used method to calculate variability. It represents the spread in glucose readings around the average.
If someone has been alternating between many highs and/or lows on a given day, their SD will be larger. In contrast, if someone has a relatively stable day, their SD will be lower. A glucose excursion can be either hyperglycemic (high blood glucose) or hypoglycemic (low blood glucose).
We can determine how frequently an individual’s blood sugar levels are significantly above or below the target/ideal range by determining the variability of blood sugar levels. Variability in glucose represents the quality of fuel and the amount of oxidative stress on your body. A blood glucose variability under 12% is considered ideal.
What Is hypoglycemia?
Hypoglycemia occurs when blood glucose falls below 70 mg/dL. It may be reactive (after meals) or fasting-related. Causes include excessive alcohol, certain medications, and metabolic disorders [Mayo Clinic, 2023].
What Is hyperglycemia?
Hyperglycemia refers to elevated blood glucose (>125 mg/dL fasting). It’s often seen in diabetes and can lead to vascular and nerve damage if chronic. Postprandial hyperglycemia is defined as levels >180 mg/dL two hours after meals
Glucose Variability and Oxidative Stress
Glucose levels at various points in time provide insight into the body’s functioning. They make for a metric that can be used to identify internal oscillations in blood glucose levels known as glucose variability. Extreme fluctuations in blood glucose levels can lead to oxidative stress in the body.
Variability in blood sugar can be caused by a variety of factors, such as a poor diet, infections, tumours, or other diseases like diabetes.
Long-term oxidative stress can cause neurodegenerative diseases, cancer and hypertension among other ailments. Monitoring glucose swings may provide actionable insight into preventing oxidative stress since the two can increase together.
How to measure Blood Glucose levels
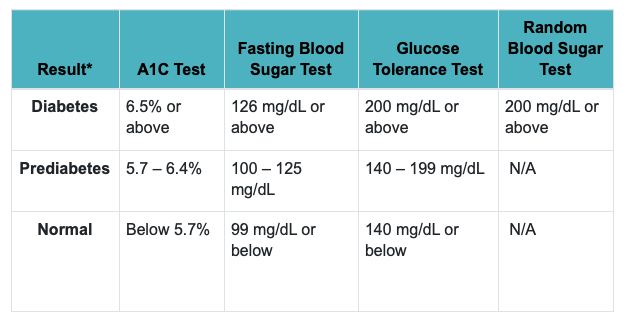
1. A1C test: A1C measures your average blood sugar levels over the past two or three months. A normal A1C level is below 5.7%, a level of 5.7% to 6.4% indicates pre-diabetes, and a level of 6.5% or more indicates diabetes.
2. Fasting blood sugar test: After an overnight fast (without eating), your blood sugar is measured. Having a fasting blood sugar level of 99 mg/dL or less is considered normal, 100 to 125 mg/dL indicates pre-diabetes, and 126 mg/dL or higher indicates diabetes.
3. Glucose tolerance test: A glucose-containing liquid is consumed before and after this device measures your blood sugar. Before the test, you will fast overnight and have your blood drawn to determine your fasting blood sugar level. After drinking the liquid, your blood sugar level will be checked for one hour, two hours, and possibly three hours later. After two hours, a blood sugar level of 140 mg/dL or lower is considered normal, 140 to 199 mg/dL indicates prediabetes, and 200 mg/dL or higher indicates diabetes.
4. Random blood sugar test: The blood sugar level is measured at the moment you are tested. It is possible to take this test at any time. You do not need to fast before taking it. Diabetes is diagnosed when your blood sugar level exceeds 200 mg/dL.
5. Post-meal glucose: Blood sugar levels are determined not only by fasting glucose but by how your body reacts to food and its ability to return to that set-point quickly. We expect glucose to rise after a meal (though if we eat carefully, it won’t rise much). If your body is not able to return to that baseline quickly, you may have insulin resistance, which prevents insulin from functioning well. We can gain some insight into that function by measuring post-meal glucose levels.
6. Continuous Glucose Monitoring (CGM):
Unlike one-time tests like fasting glucose or A1C, CGM provides real-time data on how your glucose fluctuates throughout the day. It’s especially useful for spotting post-meal spikes or nighttime lows that standard labs can miss.
CGM uses a small sensor under the skin—usually on the abdomen or arm—to track glucose in interstitial fluid. The data, sent to an app or receiver every few minutes, helps fine-tune nutrition, activity, or medication strategies.
A 2023 study found CGM more sensitive than A1C or fasting glucose in detecting early glucose issues, even in people without diabetes
Glycemic variability explained
Glycemic variability refers to the ups and downs of blood glucose levels during the day. You can only measure this with a continuous glucose monitor, which measures the interstitial fluid under your skin throughout the day.
Why monitoring blood glucose matters
Tracking your blood sugar levels helps you determine whether you’re staying within target ranges, and it can reduce symptoms of hyperglycemia (high blood sugar) and hypoglycemia (low blood sugar). Regular monitoring also reveals what causes your glucose to rise or fall — from the foods you eat to how active you are.
It’s important to note: blood sugar numbers aren’t inherently “good” or “bad.” They’re data points that offer insight into how your body responds to daily habits — and they can guide you toward better metabolic health.
Consequences of Glucose levels going unregulated
Metabolic health means maintaining optimal levels of blood glucose, triglycerides, HDL cholesterol, blood pressure, and waist circumference — without relying on medication. When these markers fall out of range, metabolic syndrome may develop, raising the risk of type 2 diabetes, heart disease, and stroke.
One of the most critical markers is blood glucose — both fasting and post-meal. While a fasting glucose under 99 mg/dL is considered normal, many experts suggest aiming for 70–80 mg/dL for better health outcomes.
Unregulated glucose leads to insulin resistance. Normally, insulin helps cells absorb sugar from the bloodstream. But constant sugar intake causes your pancreas to overproduce insulin. Eventually, cells stop responding. Blood sugar remains elevated, raising the risk of chronic disease.
Ideal range of Blood Glucose Levels Acc. Center for Disease Control and Prevention
What do blood glucose spikes at night mean?
The Somogyi effect
A drop in blood sugar overnight — often from poorly timed insulin or skipped meals — can trigger a hormonal response that leads to morning hyperglycemia. This is known as the Somogyi effect. Symptoms may include night sweats and early-morning spikes.
The Dawn Phenomenon
This spike occurs naturally in the early morning hours, as your body prepares to wake up. If blood sugar drops too low before bed, hormones like glucagon and epinephrine trigger the liver to release glucose – causing a rebound effect and elevated morning glucose.
Read our full explainer to understanding blood glucose spikes at night.
Blood glucose and athletic performance
Glucose is critical for physical performance. Athletes and those training at high intensity must keep their levels in check. If glucose drops too low, energy crashes — increasing the risk of fatigue, poor performance, or injury.
Nutrition strategies should be personalized based on sport, season, and intensity. Both carbohydrates and fats provide energy, but carbs are more readily available. Fats are more energy-dense (9 kcal/g) but slower to metabolize.
While fats and carbs can both fuel performance, carbs remain the primary fuel during high-intensity efforts. Strategic fueling — before, during, and after workouts — can improve recovery, performance, and metabolic health.

How to optimise Blood Glucose levels
1. Sleep
Poor sleep disrupts glucose metabolism. It raises cortisol, increases gluconeogenesis, and reduces glucose uptake by muscle. One study showed that just 6 days of restricted sleep elevated nighttime cortisol and growth hormone, impairing metabolic function.
2. Stress
Chronic stress triggers cortisol release — which increases blood glucose and reduces insulin sensitivity. Over time, this can impair the pancreas’s ability to regulate glucose, setting the stage for insulin resistance.
3. Exercise: Exercises like HIIT, resistance training, aerobics, and low-impact cardio are often recommended. Exercise can be segmented into vigorous/intense workouts and low/moderate intensity exercises. In anaerobic activity, glucose is broken down without oxygen being used for energy.
By using an incessant supply of oxygen, aerobic activity produces energy without any additional energy source. HIIT uses fast-twitch muscle fibres, while aerobic exercise uses slow-twitch muscle fibres.
While HIIT enhances cardio-metabolic metrics and bone formation, aerobic exercise is associated with fat metabolism. Exercise is proven to not only improve insulin sensitivity but also improve metabolic health.
4. Diet
The glycemic index (GI) ranks how quickly carbs raise blood sugar. Low-GI foods (≤55) cause smaller glucose spikes. However, GI alone doesn’t reflect a food’s healthfulness — glycemic load and nutrient density also matter.
Foods often seen as “healthy” (like oatmeal, brown rice, sweet potatoes, and fruit juice) can still spike blood sugar depending on portion size, prep method, and timing. Monitor individual responses rather than relying on general advice.
Conclusion
Glucose is the body’s primary energy source — but when levels swing wildly, it affects everything from your brain to your hormones. Over time, glucose dysregulation can lead to serious health problems. The good news? You can take control.
With the right mix of nutrition, exercise, sleep, and stress management, it’s possible to improve glucose regulation, enhance energy, and reduce long-term disease risk.
References
- Digestive System Processes – NIH
- Glycemic Variability: Can We Prevent It? – PubMed
- An Overview of Insulin – NIDDK
- Hypoglycemia – Mayo Clinic
- High Blood Sugar and Diabetes – CDC
- Blood Glucose Levels: What’s Normal? – CDC
- Glycemic Index and Glycemic Load – Harvard T.H. Chan School of Public Health
- Mediterranean Diet and Insulin Sensitivity – PubMed
- Sleep Loss and Glucose Metabolism – PubMed
- Stress, Cortisol, and Blood Sugar – Cleveland Clinic
- Exercise and Blood Glucose – ADA