Hormones are chemical signals that coordinate the way your body works. They’re produced by glands like the brain, adrenal glands, ovaries, or testes, and travel through your bloodstream to deliver instructions to different organs and tissues.
The hormone panel in Blood Vision measures a targeted set of hormones related to energy, fertility, recovery, and resilience. Many of these are shared across the male and female panels. Others, like estradiol and AMH, are specific to women’s physiology.
Read more about Blood Vision here.
Quick look: Blood Vision Hormone Panel explained
| Hormone | Panel | What it shows | What high levels may indicate | What low levels may indicate |
|---|---|---|---|---|
| Testosterone (total & free) | Male & female | Overall and active androgen levels | PCOS (in women), anabolic steroid use, tumors, low SHBG | Aging, testicular/ovarian failure, high SHBG, pituitary dysfunction |
| SHBG | Male & female | Amount of bound vs. free testosterone/estrogen | High estrogen, hyperthyroidism, liver dysfunction | Insulin resistance, obesity, hypothyroidism |
| DHEA-S | Male & female | Adrenal androgen reserve | PCOS, adrenal hyperplasia, supplement overuse | Adrenal fatigue, chronic stress, aging |
| Cortisol | Male & female | Stress response and circadian rhythm | Chronic stress, inflammation, HPA axis dysregulation | Adrenal insufficiency, burnout, pituitary suppression |
| Luteinizing hormone (LH) | Male & female | Brain–gonad signal: testosterone or ovulation trigger | PCOS, testicular/ovarian failure | Pituitary/hypothalamic dysfunction, suppressed reproductive axis |
| Follicle-stimulating hormone (FSH) | Male & female | Brain–gonad signal: sperm or egg development | Menopause, reduced ovarian/testicular function | Pituitary suppression, undernutrition, stress |
| Prolactin | Male & female | Regulation of reproductive hormone production | Stress, medications, prolactinoma | Rare, but can impair reproductive signaling |
| Estradiol (E2) | Female only | Estrogen status, menstrual cycle, mood, bone health | Estrogen dominance, tumors, PCOS | Perimenopause, ovarian failure, irregular cycles |
| Anti-Müllerian hormone (AMH) | Female only | Ovarian reserve — estimate of remaining egg supply | PCOS (many immature follicles, poor ovulation) | Reduced fertility potential, perimenopause |
Testosterone (total & free)
Testosterone is a sex hormone classified as an androgen, meaning it promotes male traits like muscle growth, facial hair, and deep voice – but it’s important in both sexes. It’s produced mainly in the testes in men and in smaller amounts by the ovaries and adrenal glands in women
- Total testosterone refers to all testosterone in the blood, including the part that’s “bound” (attached to carrier proteins like SHBG and albumin) and the “free” portion.
- Free testosterone is the fraction that is not bound to proteins and is available to enter cells and activate testosterone receptors. This is the biologically active part that actually does the work.
Why it matters:
Symptoms like fatigue, low libido, muscle loss, or poor recovery often track more closely with free testosterone, not total. That’s because high levels of SHBG can lock away too much testosterone, making it unavailable for use. A normal total level can mask a functional deficiency if your free testosterone is low.
SHBG (sex hormone–binding globulin)
SHBG is a protein made in the liver that binds tightly to sex hormones like testosterone and estradiol. When bound, these hormones are inactive – they can’t enter cells or exert effects.
Why it matters:
High SHBG means less free testosterone is available, which can lead to symptoms of low T even if your total level looks fine. SHBG tends to rise with high estrogen, thyroid hormone excess, or liver disease. Low SHBG may occur in insulin resistance, obesity, or hypothyroidism — which can increase free testosterone but also point to deeper metabolic problems.
DHEA-S (dehydroepiandrosterone sulfate)
DHEA-S is made by the adrenal gland and serves as a precursor hormone. That means it gets converted into other hormones — mainly testosterone and estrogen — in various tissues. The “S” stands for sulfate, which helps stabilize it in the bloodstream for longer-term circulation.
Why it matters:
DHEA-S gives insight into adrenal function and androgenic tone. Low levels may reflect chronic stress, aging, or poor adrenal output. Elevated levels may indicate PCOS (in women), adrenal overactivity, or overuse of DHEA supplements. It’s also useful for assessing whether your body has the raw materials to support testosterone production.
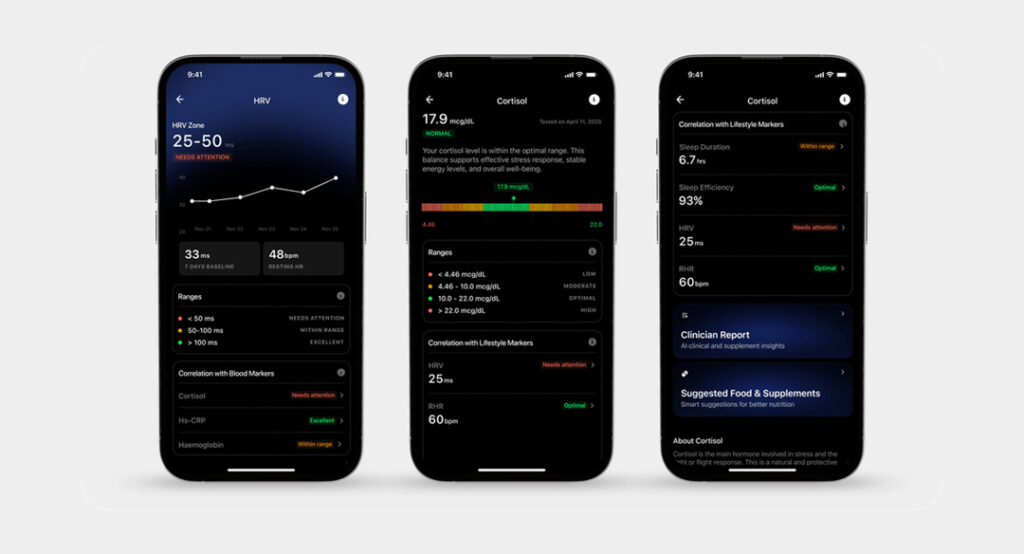
Cortisol
Cortisol is a glucocorticoid hormone made by the adrenal glands in response to stress. It’s regulated by the HPA axis — the feedback loop between your hypothalamus (brain), pituitary gland, and adrenal glands. It follows a natural rhythm: high in the morning to wake you up, low in the evening to help you wind down.
Cortisol raises blood sugar, controls inflammation, and helps your body respond to physical or emotional stress.
Why it matters:
Too much cortisol — from chronic stress, poor sleep, or overtraining — can blunt testosterone, disrupt recovery, and increase abdominal fat. Too little cortisol can leave you feeling sluggish, foggy, and fatigued. Flattened daily cortisol patterns can signal HPA axis dysfunction, sometimes referred to as adrenal fatigue.
Luteinizing hormone (LH)
LH is made by the pituitary gland, a small organ at the base of your brain. It’s triggered by GnRH (gonadotropin-releasing hormone) from the hypothalamus. LH controls reproductive hormone production:
- In men: LH stimulates Leydig cells in the testes to make testosterone.
- In women: LH spikes mid-cycle to trigger ovulation — the release of an egg from the ovary.
Why it matters:
Low LH usually means a brain-level issue — the pituitary or hypothalamus isn’t sending the right signal. High LH, in contrast, suggests the gonads (testes or ovaries) aren’t responding, so the brain keeps trying to compensate. In women, consistently high LH is often linked to PCOS. In men, it can indicate testicular damage.
Follicle-stimulating hormone (FSH)
FSH is another hormone made by the pituitary gland. It works alongside LH to regulate fertility:
- In men: FSH acts on Sertoli cells in the testes to support sperm development.
- In women: FSH helps grow and mature ovarian follicles, which eventually release an egg.
Why it matters:
FSH tells you how well the brain is communicating with the reproductive system. High levels in men may mean the testes aren’t working properly. In women, rising FSH is a classic sign of declining ovarian reserve — often seen in perimenopause. Low FSH in either sex may point to hypothalamic or pituitary suppression, possibly from stress or undernutrition.
Prolactin
Prolactin is mainly known for its role in milk production in women after childbirth. But it’s also present in men and non-pregnant women, where it helps regulate reproductive hormones
Why it matters:
High prolactin suppresses GnRH, the hormone that triggers both LH and FSH. This can lower testosterone in men and disrupt ovulation in women. Elevated prolactin is often caused by stress, certain medications (like antidepressants or antipsychotics), or a prolactinoma — a benign tumor in the pituitary gland.
Female-only hormones

Estradiol (E2)
Estradiol is the primary form of estrogen in women of reproductive age. It’s made mainly by the ovaries and plays a key role in regulating the menstrual cycle, maintaining bone density, supporting mood, and modulating fat distribution.
Why it matters:
Low estradiol can cause irregular periods, low libido, hot flashes, and bone loss. High levels might suggest estrogen dominance, which can lead to symptoms like bloating, breast tenderness, or heavy periods. Because estradiol fluctuates across the menstrual cycle, test timing is crucial — day 3 (early follicular phase) or day 21 (luteal phase) gives the most actionable data.
Anti-Müllerian hormone (AMH)
AMH is produced by granulosa cells in ovarian follicles. It reflects how many immature eggs (follicles) are still available – making it a reliable marker of ovarian reserve.
Why it matters:
AMH helps assess fertility potential, especially when planning for pregnancy or evaluating egg freezing. Low AMH suggests fewer remaining follicles, while high AMH is common in PCOS, where many follicles start to grow but don’t mature or ovulate. AMH is unique in that it stays stable throughout the cycle – so it doesn’t matter when you test it.
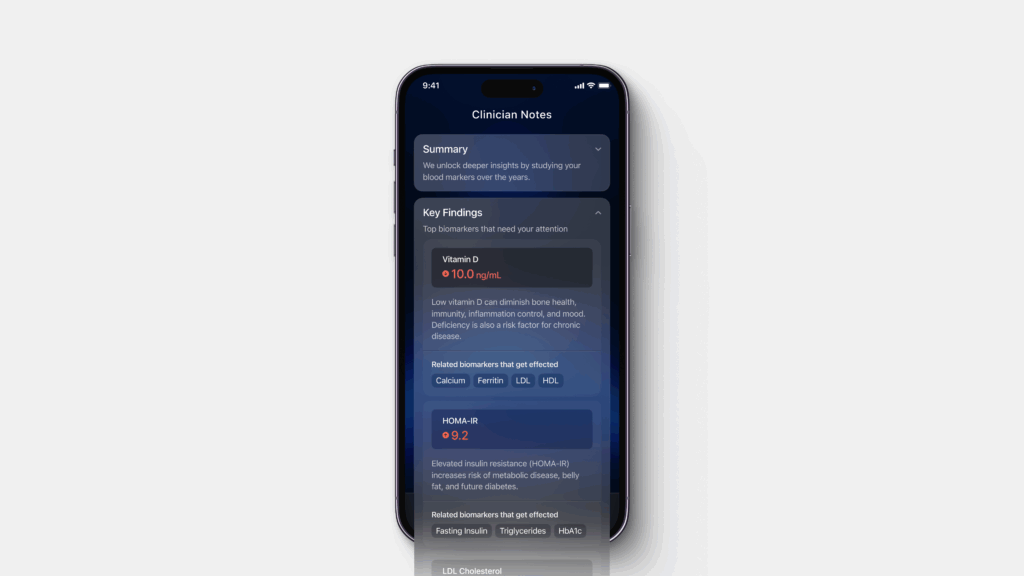
Why these hormones matter
Hormones don’t work in isolation. The levels of one hormone influence others through feedback loops between your brain, adrenal glands, and reproductive organs. For example:
- Low testosterone? Check LH and SHBG to understand the cause.
- Irregular cycles? Look at FSH, LH, estradiol, and AMH together.
- Low energy and poor recovery? DHEA-S and cortisol might hold the answer.
By measuring these key hormones together, Blood Vision helps map how your endocrine system is performing – and where intervention might help.