When it comes to health, we often jump straight into crafting a new workout routine or revamping our diet—a seemingly simple fix. Yet, the truth is, our bodies are wonderfully unique, and while exercise and good nutrition are beneficial, the key to truly optimizing your health lies in a more personalized approach.
Understanding your body’s specific needs begins with knowing where you currently stand health-wise, uncovering the internal workings of your body, and then customizing your health strategies to suit your requirements. This preventive approach is precisely where the value of blood markers lies.
What Are Blood Markers?
Blood markers, or biomarkers, are essential indicators in your blood that offer insights into your health. They come in various forms, such as cells, enzymes, hormones, or molecules, each shedding light on your health status, signaling potential diseases, or tracking the effectiveness of treatments. Doctors rely on them in the same way as blood pressure or cholesterol checks, providing a snapshot of your overall well-being and identifying any health issues before symptoms appear.
Our bodies are a complex network of systems, including the cardiovascular, metabolic, and immune systems. During a health check-up, doctors assess a variety of blood markers, such as heart rate, blood pressure, cholesterol, blood sugar, and even weight. These are comprehensive checks to help identify any risk factors for serious conditions like heart disease or diabetes, allowing for early action and better health management.
How Do Blood Markers Give You an Understanding of Your Body?
Blood markers are critical early warning signs for your health, altering you about underlying issues before they snowball into more serious conditions. These markers comprise a wide range of substances including proteins, lipids (fats), individual cells, and small molecules, each providing valuable insights into the state of your health and the functioning of your body.
For achieving peak performance, whether in athletic performance, mental acuity, or general wellness, blood markers can pinpoint areas for improvement, track progress towards health goals, and identify any underlying issues that may be hindering performance.Here are some ways blood markers can specifically help you understand your body:
- Identifying Health Issues: A lot of blood markers are directly linked to specific health conditions. For example, elevated troponin levels, a protein that is found in your heart muscles, could point to heart damage. Similarly, high alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels, which are enzymes found in the liver, can indicate liver problems. Catching health issues early on gives you a chance to get ahead of your disease, long before it has caused any lasting damage to your body.
- Monitoring Progress: Blood markers are crucial tools for tracking your health, whether you’re managing an illness or adhering to a treatment regimen.
For instance, keeping an eye on HDL (“good”) and LDL (“bad”) cholesterol levels is vital for those at risk of cardiovascular diseases. Cholesterol, a type of lipoprotein, plays a significant role in the body, including the formation of cell membranes and hormones.
However, imbalances in its levels can impact your heart, brain, and even gut health. Monitoring these markers provides a clear picture of your current health and the effectiveness of any treatment plans. By regularly checking these levels, adjustments can be made promptly, tailoring the approach to how your body is responding.
- Predicting Future Risks: Understanding your blood markers, like the levels of LDL cholesterol, is more than just a health check—it’s a forward-looking strategy deeply intertwined with longevity. Recognizing these markers early allows you to anticipate potential health challenges, particularly the risk of cardiovascular diseases. This insight empowers you to take preemptive steps, adjusting your lifestyle and diet accordingly. It’s about making informed choices today to positively influence your health tomorrow. By adopting such a proactive approach, you’re not just avoiding disease; you’re actively shaping a future where your healthspan matches your lifespan, ensuring your years are as vibrant as they are long.
- Understanding Organ Function: Understanding organ function through blood markers provides crucial insights into your health, revealing how well your organs are performing. For instance, evaluating thyroid function through markers such as Thyroid Stimulating Hormone (TSH) and thyroxine levels can highlight disorders affecting your metabolism, energy, and overall mood. This early detection is invaluable, allowing for timely interventions that can prevent minor issues from escalating into more serious health problems. By keeping a close eye on these markers, you’re not just monitoring your health; you’re actively taking steps to maintain and improve it, emphasizing the role of regular blood analysis in comprehensive health management.
Keeping track of these markers over time paints a detailed picture of your health trends. This continuous insight empowers you to make informed decisions regarding your lifestyle, diet, and healthcare, keeping you engaged and proactive about your well-being.

Blood Vision: Revolutionizing Preventive Blood Testing
Blood Vision introduces a new approach to preventive blood testing through its UltraTrace™ technology. This advancement is not just another blood test; it marks a significant step forward in health and wellness monitoring.
UltraTrace™ technology innovatively links changes in sleep patterns, resting heart rate, heart rate variability, and physical activity with key blood markers, based on decades of comprehensive research.
For instance, UltraTrace™ can analyze the impact of improved sleep quality on a blood marker such as LDL, giving users a probability score. This functionality provides a clearer understanding of how lifestyle habits directly influence blood markers.
By enabling users to track their health markers over time, Blood Vision provides personalized insights through advanced algorithms. This approach prioritizes longevity and proactive well-being, marking a departure from traditional disease-centric metrics and emphasizing preventive healthcare.
Below, we’ll explore the markers measured to deliver a full spectrum of insights into your health:
General Health Parameters
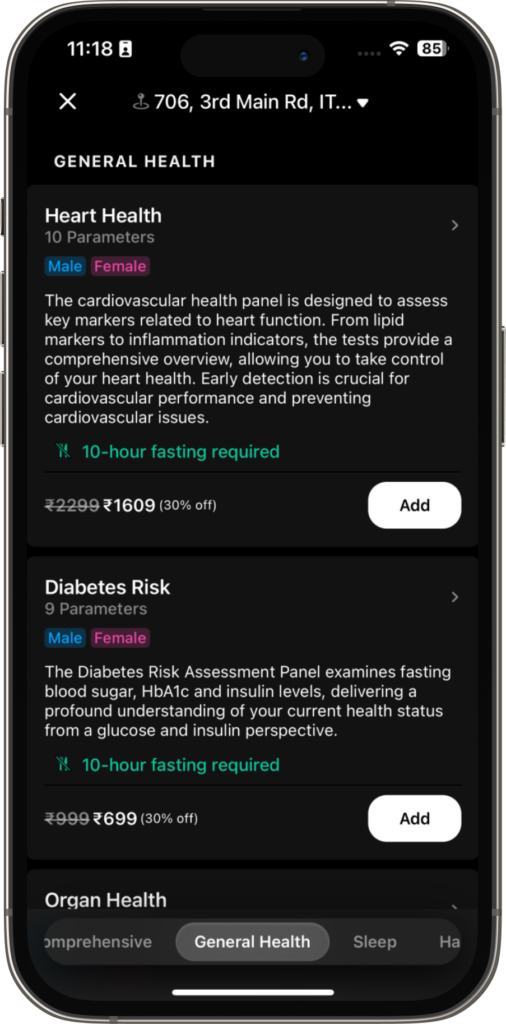
Heart Health
The cardiovascular or heart health panel is an invaluable tool for the early detection and management of conditions affecting the heart. By evaluating a range of critical markers, including lipid profiles and signs of inflammation, this comprehensive test provides an in-depth look at heart function. Recognizing these markers allows you to take proactive measures in safeguarding your heart health, thereby enhancing cardiovascular performance and preventing potential issues. Let’s examine the markers included in this panel, focusing solely on their importance for heart health.
- Hs-CRP (High-sensitivity C-reactive Protein):
The liver produces High-sensitivity C-reactive Protein (hs-CRP) in response to inflammation, making it a crucial marker for detecting inflammation levels in the body. Various triggers can cause this protein’s levels to rise, indicating potential health issues, including cardiovascular disease risk. An increase in hs-CRP levels points to a higher risk of heart disease, as chronic inflammation plays a significant role in atherosclerosis development—a condition characterized by plaque buildup in the arteries, which could lead to heart attacks or strokes. Therefore, monitoring hs-CRP levels is vital for assessing heart health and guiding interventions to prevent cardiovascular complications. - Homocysteine:
Homocysteine, an amino acid in the bloodstream, is a crucial marker for health. High levels can indicate an increased risk for heart conditions and point to deficiencies in vital B vitamins—B6, B9 (folate), and B12—which are essential for DNA repair and various cellular functions. Furthermore, elevated homocysteine can disrupt methylation, a critical process involved in DNA repair, detoxification, energy production, and immune function. This disruption can impact everything from energy levels to cellular repair mechanisms. Therefore, monitoring and managing homocysteine levels is vital not only for cardiovascular health but also for supporting the body’s essential functions and overall well-being. - Apolipoprotein A1 (ApoA1) and Apolipoprotein B (ApoB):
These proteins play a key role in lipid (fat) metabolism. ApoA1 is associated with HDL (high-density lipoprotein), or “good” cholesterol, promoting the removal of cholesterol from the bloodstream and thus protecting against heart disease. On the other hand, ApoB is a primary component of LDL (low-density lipoprotein) and VLDL (very-low-density lipoprotein), known as “bad” cholesterols, because they can lead to plaque buildup in arteries, increasing heart disease risk. Together, these markers offer insights not just into cardiovascular health but also your broader metabolic health, including the risk of developing conditions like metabolic syndrome, which encompasses a cluster of symptoms associated with increased heart disease, stroke, and diabetes risk. - Lipoprotein (a) [Lp(a)]:
Lipoprotein (a), or Lp(a), is a type of particle in your blood that carries cholesterol, fats, and proteins. It’s similar to LDL, often called “bad” cholesterol, because it can build up in the walls of arteries, leading to clogged arteries. What makes Lp(a) unique is the additional protein it carries, which makes it even more effective at sticking to artery walls and can significantly increase the risk of heart disease. High levels of Lp(a) are not only linked to a greater chance of developing heart conditions but also to an increased risk of thrombosis, which means forming dangerous blood clots in veins or arteries. Given its role in heart and vascular health, keeping an eye on Lp(a) levels is crucial in preventing cardiovascular diseases and ensuring the health of your blood vessels. - Total Cholesterol, Triglycerides, LDL Cholesterol, VLDL Cholesterol, and HDL Cholesterol:
These lipid markers collectively provide a snapshot of heart disease risk. Total cholesterol encompasses all types of cholesterol in the blood; a balanced level is crucial for good health. Triglycerides, a type of fat, when high, can indicate poor metabolic health and an increased risk of cardiovascular disease. LDL and VLDL cholesterol are considered “bad” because they contribute to plaque buildup in arteries, whereas HDL cholesterol is “good” as it helps remove other forms of cholesterol from the bloodstream. Monitoring these markers offers a comprehensive view of how your body manages fats, which is influenced by diet, hormones, and liver function. This insight is invaluable for assessing not only cardiovascular health but also overall metabolic wellness.
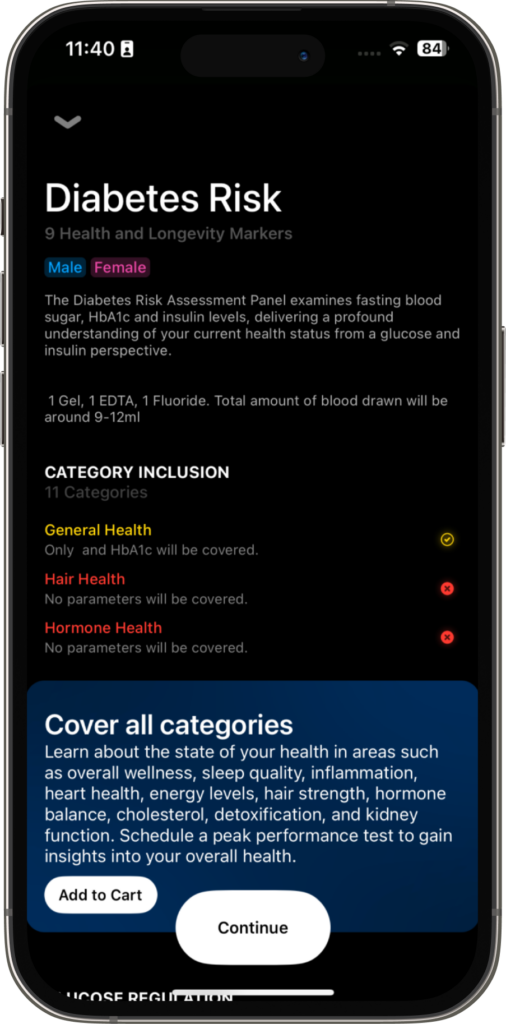
Diabetes Risk Assessment
The diabetes risk assessment panel is crucial because it helps identify the likelihood of developing diabetes—a condition that, when unmanaged, can result in severe complications like heart disease, kidney failure, and vision impairment. By tracking important markers such as fasting blood sugar, HbA1c, and insulin levels, you gain valuable insights into how effectively your body regulates glucose. Managing or preventing diabetes is essential for averting these complications and promoting a longer, healthier life. Understanding these markers plays a vital role in sustaining balanced glucose levels and lowering the risk of diabetes. Let’s explore the markers included in this panel:
- Glucose Regulation Metrics:
- Fasting Glucose: The fasting glucose test is a blood test that measures your blood sugar levels after you’ve fasted (not eaten) for at least 8 hours. It’s crucial because high levels can indicate that your body is not effectively managing blood sugar, which is a sign of diabetes. Maintaining blood sugar within a healthy range is essential for managing energy levels, mood, and general health, making this test significant for identifying potential health issues and preventing complications associated with diabetes.
- Fasting Insulin:
The fasting insulin test measures the levels of insulin, a vital hormone for utilizing or storing blood sugar, in your blood after you’ve fasted for a certain period. High insulin levels may indicate that your body is starting to resist the effects of insulin, often a precursor to developing type 2 diabetes. Since insulin plays a key role in maintaining energy stability and minimizing the risk of metabolic diseases, this test is important for detecting early signs of insulin resistance and preventing the progression towards diabetes. - HbA1c (Hemoglobin A1c):
The HbA1c test measures your average blood sugar levels over the past few months, providing a window into how well your body manages blood sugar over time. Elevated HbA1c levels indicate persistent blood sugar control problems, playing a crucial role in diagnosing and managing diabetes. Keeping blood sugar levels stable is key to avoiding long-term damage to organs and tissues, making this test an important tool for monitoring and safeguarding your health. - HOMA IR (Homeostatic Model Assessment of Insulin Resistance):
The HOMA IR test calculates your body’s insulin resistance using fasting glucose and insulin levels, offering insight into how well your body uses sugar for energy. High scores indicate insulin resistance, a precursor to type 2 diabetes. This test is crucial for identifying early signs of metabolic issues, and guiding interventions to improve sugar utilization and energy management, thereby preventing diabetes progression.
- Fasting Glucose: The fasting glucose test is a blood test that measures your blood sugar levels after you’ve fasted (not eaten) for at least 8 hours. It’s crucial because high levels can indicate that your body is not effectively managing blood sugar, which is a sign of diabetes. Maintaining blood sugar within a healthy range is essential for managing energy levels, mood, and general health, making this test significant for identifying potential health issues and preventing complications associated with diabetes.
Cholesterol Assessment Metrics
- Total Cholesterol: The Total Cholesterol test measures the overall level of cholesterol in your blood. Although not directly related to diabetes, high cholesterol is a significant risk factor for cardiovascular disease—a condition often worsened by diabetes. Monitoring and managing cholesterol levels are vital for maintaining heart health and preventing blockages in the arteries.
- Triglycerides: The Triglycerides test measures the levels of a specific type of fat in your blood. High triglyceride levels indicate a build-up of fat in your arteries, signaling an increased risk for cardiovascular disease and indicating insulin resistance, a condition related to type 2 diabetes. Managing triglyceride levels is essential for maintaining metabolic health and lowering the risk of heart disease, highlighting the importance of this test in a comprehensive health assessment.
- LDL (Low-Density Lipoprotein): The LDL test measures levels of low-density lipoprotein in your blood, often referred to as “bad” cholesterol. High LDL levels can cause plaque buildup in the arteries, elevating the risk of heart disease. For individuals with diabetes, managing LDL becomes even more critical to prevent cardiovascular complications. Understanding your LDL levels is crucial for taking preventive measures against artery blockage and maintaining heart health, especially important for those at increased risk due to diabetes.
- VLDL (Very-Low-Density Lipoprotein): The VLDL test checks for a type of fat called very-low-density lipoprotein in your blood, which carries triglycerides. Just like “bad” cholesterol, high VLDL can increase your risk of heart disease. It’s often high in people with diabetes, showing how crucial it is to keep an eye on fat levels for your overall health. By keeping track of VLDL, you can take steps early to protect your heart, especially important for anyone with diabetes.
- HDL (High-Density Lipoprotein): The HDL test measures the level of high-density lipoprotein in your blood, known as “good” cholesterol. HDL helps clear other forms of cholesterol from your bloodstream. Low levels of HDL are worrisome, particularly for individuals with diabetes, because they can increase the risk of cardiovascular disease. Keeping an eye on your HDL levels is crucial because it plays a key role in keeping your heart healthy by helping to prevent the buildup of bad cholesterol.
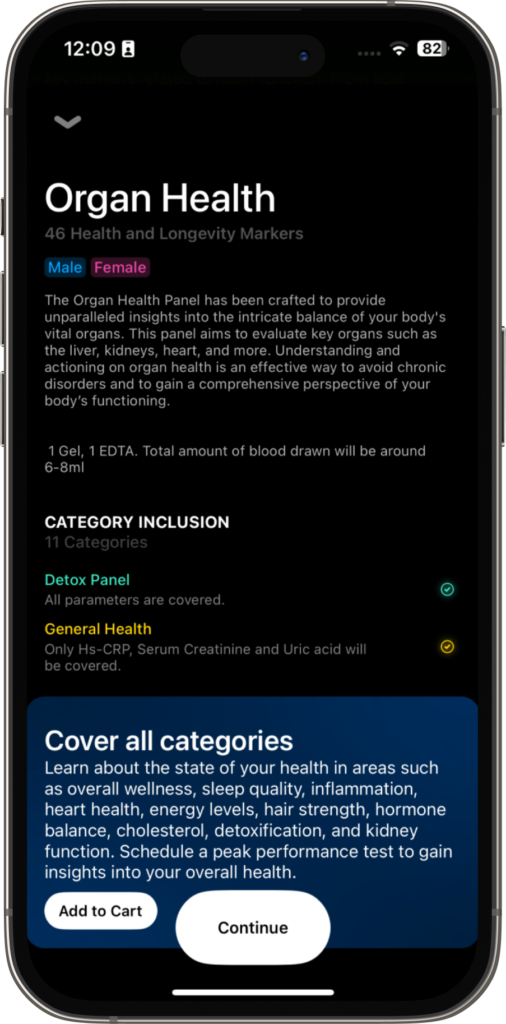
Organ Health Panel
The Organ Health Panel is a comprehensive test that assesses the health and function of your body’s crucial organs. By measuring various biomarkers proactively, it aims to understand overall well-being and uncover any potential concerns before they develop further. This panel is essential for managing health conditions and offers a broad perspective on your well-being, contributing to longevity through early detection and intervention. This approach supports the long-term health of your vital organs, helping maintain health and enhance life quality over the years. Let’s elaborate on the key components of this panel:
- Serum Creatinine: This is a byproduct of muscle metabolism, typically filtered out by the kidneys. Elevated serum creatinine levels can indicate that the kidneys are not functioning properly, suggesting potential kidney damage or chronic kidney disease. This marker is also essential because kidney function is closely tied to the overall health of other organs. Efficient kidneys help manage blood pressure, filter waste, and balance electrolytes, which in turn supports heart health, bone strength, and the proper function of muscles and nerves, safeguarding your overall health.
- Uric Acid: High levels of uric acid in the blood can result from the body breaking down purines found in certain foods or the inability of the kidneys to adequately eliminate uric acid. This condition can lead to gout, arthritis and/or kidney stones, highlighting issues with kidney function or metabolic disorders. This condition not only signals the potential for gout, arthritis, and kidney stones but also serves as a marker for underlying kidney function issues or metabolic disorders. Monitoring uric acid levels is crucial in identifying risks early on, allowing for interventions that can prevent these conditions from worsening or even developing. For instance, a buildup of uric acid can affect cardiovascular health, contributing to hypertension and an increased risk of heart disease. It can also impact the endocrine system, particularly in how the body regulates blood sugar and fat metabolism.
- Hs-CRP (High-sensitivity C-reactive Protein): As seen earlier, High-sensitivity C-reactive Protein (hs-CRP) measures inflammation. Chronic inflammation can severely undermine the health of every organ in your body. It acts as a common thread linking numerous diseases, from heart disease where it promotes atherosclerosis, to the brain where it’s associated with neurodegenerative disorders to even liver health where it can cause fatty liver disease.
- Electrolytes (Potassium, Chloride, Sodium): Electrolytes like potassium, chloride, and sodium are crucial for your body’s functions, including nerve signaling and muscle contraction, which directly affect physical performance and overall health. Imbalances in these electrolytes can indicate kidney issues since the kidneys are responsible for keeping electrolyte levels in check. For athletes and anyone engaging in physical activities, maintaining balanced electrolyte levels is vital for optimal performance, as they help prevent muscle cramps and fatigue. Proper electrolyte management can enhance endurance, strength, and recovery, making it essential for peak physical condition and health.
- Thyroid Panel (Free T3, Free T4, TSH): The Thyroid Panel, including Free T3, Free T4, and TSH tests, checks the health of your thyroid gland by measuring levels of thyroid hormones. These hormones are pivotal for many body functions, such as metabolism, heart rate, and temperature control. For instance, hypothyroidism (underactive thyroid gland) can slow metabolism, contributing to weight gain and decreased energy, and affect heart health by lowering heart rate and raising cholesterol levels. Conversely, hyperthyroidism (overactive thyroid gland) accelerates metabolism, causing weight loss and potentially leading to an increased heart rate and higher blood pressure. These imbalances underscore the thyroid’s critical role in ensuring the efficient function and health of various organs, highlighting the importance of maintaining thyroid health for overall well-being.
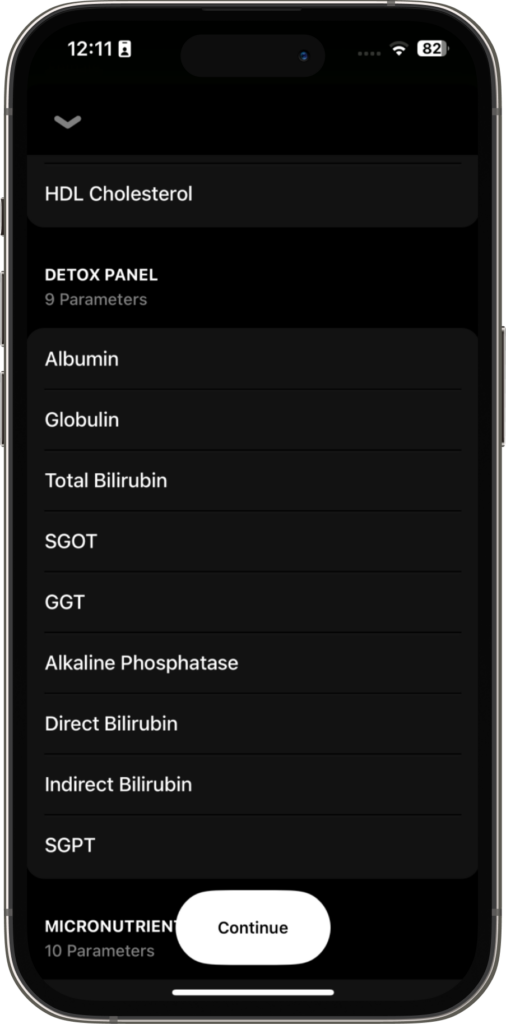
- Liver Function Tests (Albumin, Globulin, Total Bilirubin, Direct Bilirubin, Indirect Bilirubin, SGOT, SGPT, GGT, Alkaline Phosphatase): Liver Function Tests measure key markers like Albumin, Bilirubin, and enzymes (SGOT, SGPT, GGT, Alkaline Phosphatase) to check your liver’s health. This organ plays crucial roles in filtering toxins, helping digest food, and processing medications. If these test levels are off, it might mean your liver is inflamed, damaged, or not working properly. This could impact your overall health, from feeling more tired to not processing drugs effectively. Keeping an eye on these levels helps catch liver issues early, ensuring you can take steps to keep your liver healthy and your body running smoothly.
- Lipid Panel (Total Cholesterol, Triglycerides, LDL, HDL, VLDL): The Lipid Panel, as we have seen earlier, is essential because it measures fats in your blood, like cholesterol and triglycerides. All of these are vital for organ health, particularly for your cardiovascular health. Imbalanced lipid levels can also affect the pancreas, potentially leading to pancreatitis, and impact brain health, with high LDL cholesterol linked to an increased risk of neurological disorders. These effects underscore the importance of lipid management for the health of multiple organs.
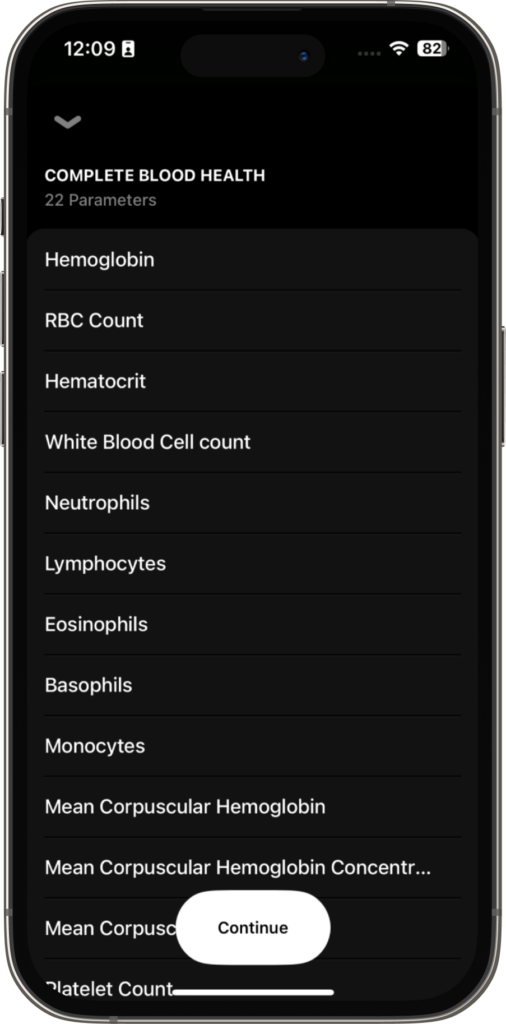
Complete Blood Health
- Hemoglobin, RBC Count, Hematocrit: Hemoglobin, RBC Count, and Hematocrit levels are crucial because they indicate the blood’s capacity to carry oxygen, which is essential for both health and performance. Adequate oxygen delivery to tissues is necessary for optimal organ function, energy production, and overall vitality. Inadequate levels of these values, indicative of conditions like anemia, can lead to fatigue, weakness, and decreased physical and cognitive performance. Monitoring and maintaining optimal levels ensure that the body receives enough oxygen to support cellular metabolism and sustain peak performance in daily activities, exercise, and cognitive tasks, contributing to both health and performance optimization
- White Blood Cell (WBC) Count and Differential: The White Blood Cell (WBC) Count and Differential tests help gauge the body’s immune response. Changes in WBC counts, whether elevated or decreased, can signal various conditions like infections, inflammation, or autoimmune diseases. This is important because the immune system defends the body against illnesses, and irregular WBC counts can affect multiple organs and functions. Monitoring immune status helps catch health issues early, allowing for timely management and ensuring the body stays resilient against infections and other threats. Maintaining a healthy immune response is key to overall well-being and effective disease prevention.
- Mean Corpuscular Volume (MCV), Mean Corpuscular Hemoglobin (MCH), and Mean Corpuscular Hemoglobin Concentration (MCHC): Mean Corpuscular Volume (MCV), Mean Corpuscular Hemoglobin (MCH), and Mean Corpuscular Hemoglobin Concentration (MCHC) are indices that offer insights into the size and hemoglobin content of red blood cells. They aid in diagnosing various types of anemia, a condition that can affect the oxygenation and function of organs. This is crucial because adequate oxygen delivery to tissues is essential for optimal organ function and overall health. Monitoring these indices helps identify anemia early and allows for appropriate interventions to restore normal red blood cell parameters, ensuring adequate oxygen supply to tissues and maintaining optimal organ function.
- Platelet Count: Platelet Count is essential for both health and performance. Adequate platelets are necessary for proper blood clotting, preventing excessive bleeding or inappropriate clot formation, which can jeopardize health and lead to organ damage. For peak performance, optimal platelet function ensures efficient oxygen delivery during physical activity and aids in tissue repair post-exercise. Monitoring platelet counts is crucial for maintaining overall health and optimizing physical performance by safeguarding against clotting disorders and promoting efficient blood circulation.
- Mentzer Index, Sehgal Index, ESR (Erythrocyte Sedimentation Rate): The Mentzer Index and Sehgal Index help differentiate between different types of anemia, providing insight into the underlying causes of low red blood cell count. For example, the Mentzer Index can help distinguish between iron deficiency anemia, a condition wherein there are too few healthy red blood cells due to too little iron in the body. and thalassemia, a genetic blood disorder caused when the body doesn’t make enough of a protein called hemoglobin. The Sehgal Index is useful in identifying iron deficiency anemia.
On the other hand, the Erythrocyte Sedimentation Rate (ESR) measures the rate at which red blood cells settle in a tube over time. An elevated ESR can indicate the presence of inflammation in the body, which may be associated with various conditions such as infections, autoimmune diseases, or cancer.
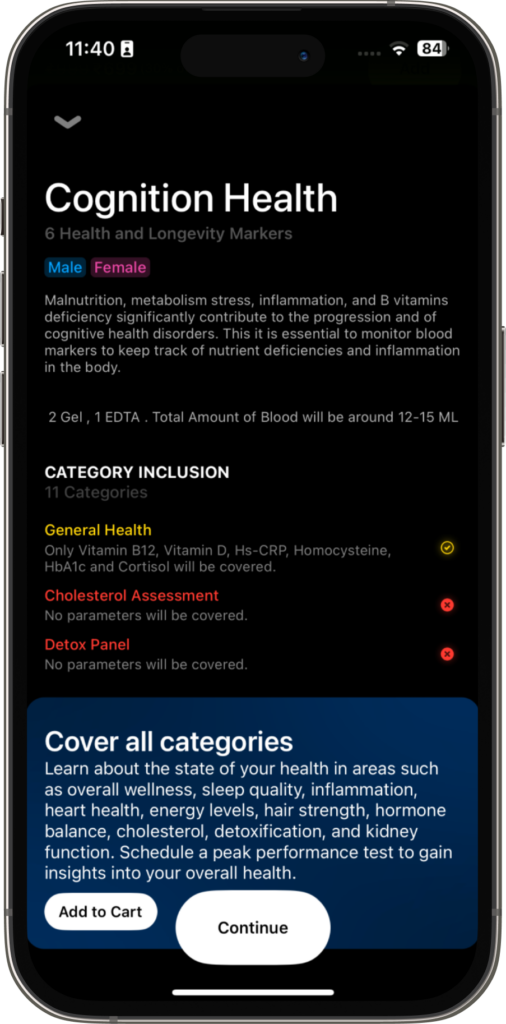
Cognition Health Panel
The Cognition Health Panel is specifically designed to monitor key blood markers that play a significant role in the development and progression of cognitive health disorders. Factors such as malnutrition, metabolic stress, inflammation, and deficiencies in essential vitamins, particularly B vitamins, can adversely affect cognitive function. By keeping track of these markers, it’s possible to gain insights into nutrient deficiencies and inflammatory states in the body, which are crucial for maintaining cognitive health and preventing disorders such as dementia. Let’s look at the core metrics and their implications for cognitive health:
- Vitamin B12: Vitamin B12 is vital for nerve function, brain health, and the production of DNA and red blood cells. A deficiency in Vitamin B12 can lead to cognitive issues, memory problems, and neurological changes.
- Vitamin D: While often associated with bone health, Vitamin D also plays a critical role in brain health and function. Low levels of Vitamin D have been linked to an increased risk of cognitive decline and dementia.
- Hs-CRP (High-sensitivity C-reactive Protein): As seen, this marker indicates inflammation in the body. Chronic inflammation is associated with a higher risk of cognitive decline and disorders such as Alzheimer’s disease.
- Homocysteine: Elevated levels of this amino acid are a risk factor for brain diseases, including dementia and Alzheimer’s disease. High homocysteine can indicate B vitamin deficiencies and is harmful to brain health.
- HbA1c (Hemoglobin A1c): This marker provides an average blood sugar level over the past two to three months. High HbA1c levels are associated with an increased risk of cognitive decline, as consistent high blood sugar can damage blood vessels in the brain.
- Cortisol: Known as the stress hormone, elevated cortisol levels over a prolonged period can impair cognitive functions such as memory and learning. Chronic stress, leading to high cortisol, has been linked to brain structure changes and cognitive decline.
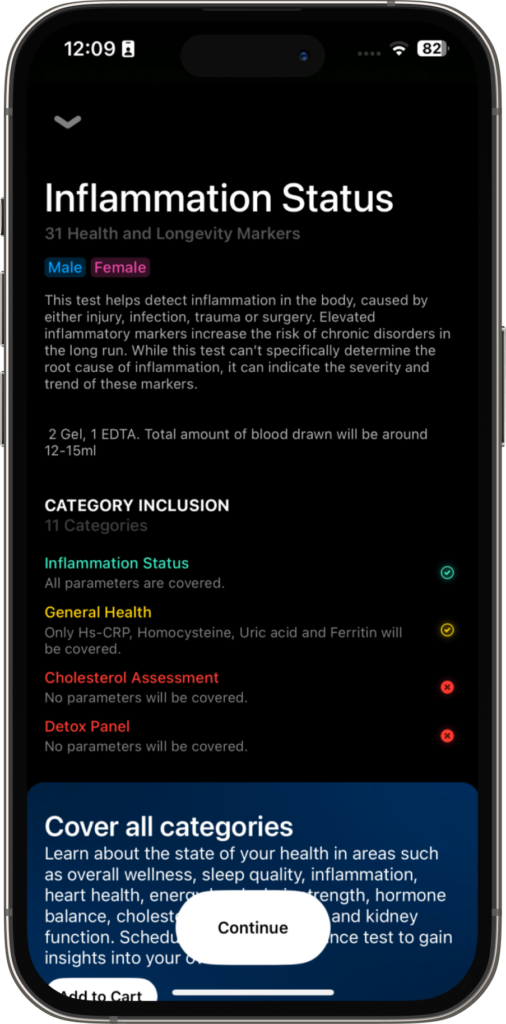
Inflammation Status Panel
This panel methodically evaluates a series of markers to gauge the body’s inflammatory response, which plays a significant role in overall health and well-being. Chronic inflammation serves as a connecting factor among numerous health conditions, including cardiovascular diseases, autoimmune disorders, and more. Delving into how each marker relates to inflammation and general health can illuminate potential health risks and areas needing attention. Here’s an overview of how these markers connect to inflammation and health:
- Homocysteine: Homocysteine is an essential amino acid produced during the metabolism of methionine. Elevated levels of homocysteine are associated with inflammation and oxidative stress, leading to damage to blood vessel walls and promoting atherosclerosis, the buildup of plaque in arteries. This contributes to cardiovascular disease risk and systemic inflammation.
- High-sensitivity C-reactive Protein: When this marker is high, it shows there are signs of on-going inflammation affecting your entire body, making you more susceptible to chronic diseases.
- Erythrocyte Sedimentation Rate: SR measures the rate at which red blood cells settle in a tube of blood over time. Elevated ESR indicates the presence of inflammation, as inflammatory proteins cause red blood cells to clump together and settle faster. An increased rate here may signify systemic inflammation. A high erythrocyte sedimentation rate is often associated with a variety of conditions, including infections, autoimmune diseases, and chronic inflammatory states, reflecting widespread inflammation.
- Fasting Insulin: Elevated fasting insulin levels can serve as a subtle yet significant indicator of underlying inflammation, pointing to insulin resistance before other symptoms manifest. This relationship highlights the interconnectedness between metabolic dysfunction and inflammation, with insulin resistance not only contributing to metabolic disturbances but also signaling broader inflammatory processes. Recognizing fasting insulin as an inflammation marker allows for early intervention
- Uric Acid: Uric acid is a waste product formed during the breakdown of purines in the body. Elevated uric acid levels can result from increased production or decreased excretion, leading to the formation of urate crystals and triggering inflammation. High levels of uric acid can lead to gout or arthritis, both inflammatory conditions. Additionally, elevated uric acid is linked with broader inflammation in the body and can increase the risk of chronic disease development.
- Ferritin: While ferritin is a marker for iron storage, elevated levels can be indicative of inflammation or infection. High ferritin levels are commonly seen in states of inflammation and can be a sign of chronic disease or an acute inflammatory response.
- Immunoglobulin E: IgE is an antibody produced by the immune system in response to allergens. Allergic reactions trigger the release of IgE, leading to the release of inflammatory mediators such as histamine, which causes allergy symptoms. High levels of Immunoglobulin E can indicate allergic reactions, which are inflammatory responses to perceived threats by the immune system.

Complete Blood Count
- Hemoglobin, Red Blood Cell Count, Hematocrit: Hemoglobin is a protein in red blood cells that carries oxygen from the lungs to the body’s tissues. Red blood cell count refers to the number of red blood cells per volume of blood, while hematocrit measures the percentage of blood volume occupied by red blood cells. Conditions like anemia, often identified through these markers, can result from or cause chronic inflammation. Chronic diseases that lead to inflammation can disrupt the normal production of red blood cells.
- White Blood Cell Count and Differential (Neutrophils, Lymphocytes, Eosinophils, Basophils, Monocytes): White blood cells (WBCs) are key components of the immune system, defending the body against infections and inflammation. An increase in white blood cells and shifts in their proportions can signal an immune response to inflammation or infection, indicating the body’s stress or response to inflammatory stimuli.
- Platelet Count: Platelets are blood cells involved in clotting and wound healing. Abnormal platelet counts can be linked to various inflammatory diseases and conditions. Particularly, an elevated platelet count often occurs in response to inflammation.
- Mean Corpuscular Hemoglobin, Mean Corpuscular Hemoglobin Concentration, Mean Corpuscular Volume: These indices shed light on red blood cell characteristics. Deviations from the norm can indicate conditions like anemia, which may be related to or a result of inflammation. Inadequate oxygen delivery to muscles can impair exercise performance, leading to fatigue, reduced endurance, and diminished physical capacity
- Mentzer Index, Sehgal Index: These specific indices assist in diagnosing different types of anemia, which can be associated with or a consequence of chronic inflammation and nutritional deficiencies. Fatigue and weakness resulting from anemia can compromise physical performance, reducing endurance, strength, and overall athletic ability.

Sleep Status
Understanding your sleep deeply is crucial for overall health, as it impacts various aspects of well-being. Several markers influence your sleep-wake cycle and can offer insights into your sleep quality, which in turn affects all aspects of your health. These markers include Vitamin D, Cortisol, Magnesium, Ferritin, Iron, Fasting Glucose, HbA1c, Hs-CRP, TSH, Free T3, and Free T4. By monitoring and optimizing these markers, individuals can enhance their sleep quality, support physical recovery, and improve cognitive function, ultimately leading to better health and performance. Here are the blood markers we test in the sleep status panel:
- Vitamin D: Vitamin D has a connection with both sleep quality and the body’s circadian rhythm. Adequate levels of this vitamin don’t just bolster bone health and immune function but also play a pivotal role in how well we sleep and how our internal clock operates. The presence of vitamin D receptors in the brain areas responsible for managing our sleep-wake cycles hints at its importance in ensuring our sleep is restorative and in harmony with our natural rhythm. This harmonious sleep cycle is crucial for our daily recovery, mental sharpness, and overall vitality. In essence, maintaining optimal vitamin D levels can be seen as a key factor not only for our physical health but also for ensuring we get quality sleep, which in turn, supports our day-to-day performance and well-being.
- Cortisol: Cortisol regulates metabolism, stress response, and the sleep-wake cycle. Balanced cortisol levels are essential for energy production, stress management, and maintaining a healthy sleep pattern. Optimizing cortisol levels can improve stress resilience, mental clarity, and sleep quality. This hormone, often dubbed the “stress hormone,” has a natural rhythm that ideally peaks in the morning to help us wake up and gradually decreases throughout the day, reaching its lowest levels at night to facilitate sleep. When cortisol levels are balanced, they foster a state conducive to restful sleep, allowing for proper recovery and rejuvenation of the mind and body. However, when this balance is disrupted, either by stress, irregular schedules, or other factors, it can lead to difficulties in falling asleep or staying asleep, impacting overall sleep quality.
- Magnesium: Magnesium is involved in hundreds of biochemical reactions in the body, including energy production, muscle function, and nerve transmission. Adequate magnesium levels are essential for overall health and vitality. Optimizing magnesium levels supports muscle relaxation, nerve function, and energy metabolism, reducing the risk of muscle cramps, fatigue, and stress-related symptoms. This can improve physical endurance, mental clarity, and sleep.
- Ferritin: Ferritin levels have a significant connection to sleep quality and overall sleep health. Iron, stored and regulated by ferritin, plays a critical role in the production of dopamine, a neurotransmitter that, among other things, helps regulate sleep. Low ferritin levels can lead to iron deficiency, which may disrupt sleep patterns, contribute to restless leg syndrome—a condition that causes an irresistible urge to move the legs, often disrupting sleep—and increase the likelihood of insomnia or unrefreshing sleep. Furthermore, adequate iron levels are essential for maintaining the energy levels necessary for optimal daily functioning, which is influenced by the quality of sleep. Thus, ensuring ferritin levels are within a healthy range not only supports physical and cognitive functions but also promotes better sleep quality, which is crucial for overall well-being and performance.
- Iron: Adequate iron levels play a critical role in sleep health by supporting effective oxygen transport and reducing the risk of conditions like restless leg syndrome, which can disrupt sleep. Optimizing iron levels can improve sleep quality by ensuring proper oxygen delivery to tissues and alleviating symptoms that interfere with restful sleep, such as the discomfort and urge to move associated with restless leg syndrome. This contributes to better overall well-being by allowing for more restorative sleep.
- Fasting Glucose: Balanced fasting glucose levels have a significant impact on sleep quality. Stable blood glucose through the night supports uninterrupted sleep, as fluctuations can cause awakenings or disturbances in the sleep cycle. Low overnight glucose levels can lead to hypoglycemia, which may cause discomfort and awakenings, while high levels, indicative of poor glucose control, can lead to symptoms like thirst and frequent urination, disrupting sleep. Furthermore, good glucose regulation supports energy levels and cognitive function upon waking, contributing to overall feelings of restfulness and readiness for the day. Optimizing fasting glucose levels, therefore, not only reduces the risk of diabetes and supports daytime functioning but also plays a key role in ensuring restorative sleep.
- HbA1c (Hemoglobin A1c): Maintaining balanced HbA1c levels is also crucial for sleep health, as it reflects long-term glucose stability, which influences sleep quality. Consistent blood sugar levels help prevent sleep disruptions that can occur with glucose fluctuations, such as waking up during the night feeling hungry or needing to urinate, both common in uncontrolled diabetes. Moreover, well-regulated HbA1c levels reduce the risk of conditions like sleep apnea, which is more prevalent in individuals with diabetes, further emphasizing the importance of good glucose control for uninterrupted and restorative sleep. By optimizing HbA1c levels, you support not just daytime energy and cognitive function but also contribute to the foundation of good sleep.
- Hs-CRP: Balanced levels of hs-CRP, indicating well-managed inflammation, play a significant role in sleep health. Chronic inflammation can disrupt sleep by affecting the body’s ability to enter deep, restorative sleep phases, potentially leading to insomnia or poor sleep quality. Elevated hs-CRP levels are associated with an increased risk of sleep disorders, including sleep apnea, which not only disrupts sleep but also further exacerbates inflammation, creating a cycle that can be hard to break. By optimizing inflammation levels, and thereby lowering hs-CRP, you can help ensure more restful, uninterrupted sleep. This, in turn, supports the body’s healing processes, immune function, and overall well-being.
- Thyroid-Stimulating Hormone (TSH): Optimizing Thyroid-Stimulating Hormone (TSH) levels is pivotal for sleep quality due to its regulatory role in thyroid function, which impacts metabolism and energy levels. Imbalances in TSH, indicating either hypothyroidism or hyperthyroidism, can significantly affect sleep patterns. Elevated TSH levels, signaling hypothyroidism, may lead to difficulties in staying asleep and an increased need for sleep, contributing to daytime fatigue. On the other hand, low TSH levels, indicative of hyperthyroidism, can cause insomnia or reduced sleep quality due to heightened metabolism and energy levels, making it difficult to fall asleep or maintain a deep sleep state. By maintaining balanced TSH levels, one supports not only metabolic balance and energy production throughout the day but also contributes to the foundation of restorative sleep.
- Free Triiodothyronine (Free T3): Optimal levels of Free Triiodothyronine (Free T3) are crucial for maintaining a healthy sleep cycle, given its significant role in regulating metabolism, energy production, and body temperature. When Free T3 levels are balanced, the body’s metabolic rate is optimized, which is conducive to better sleep quality. Abnormal Free T3 levels can disrupt these processes, leading to sleep disturbances. For example, elevated Free T3 levels can increase metabolism and body heat production, potentially causing difficulties with falling asleep or staying asleep.
- Free Thyroxine (Free T4): Balancing Free T4 levels plays a pivotal role in ensuring quality sleep by maintaining a steady metabolic rate and energy balance. When Free T4 is in harmony, it fosters a conducive environment for restful sleep, preventing the metabolic disturbances that can cause sleep difficulties. Conversely, imbalances may disrupt sleep, affecting both the ease of falling asleep and the depth of sleep achieved. Therefore, keeping Free T4 levels well-regulated is vital for not just metabolic health but also for supporting restorative sleep essential to overall vitality.
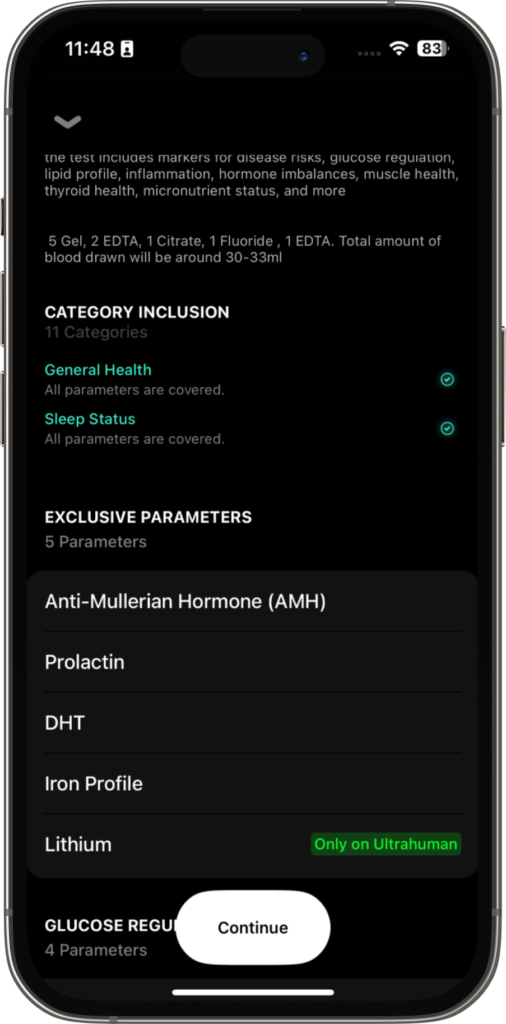
Exclusive parameters
- AMH (Anti-Müllerian Hormone): AMH is primarily associated with ovarian reserve and can help assess fertility potential in women. Monitoring AMH levels aids in understanding reproductive health and fertility status. Low AMH levels may indicate a reduced ovarian reserve, suggesting diminished fertility potential and a higher risk of infertility or difficulty conceiving. High AMH levels may be associated with conditions such as polycystic ovary syndrome (PCOS), which can disrupt menstrual cycles and ovulation, affecting fertility. Optimizing AMH levels can guide fertility treatments and family planning decisions.
- Prolactin: Prolactin is a hormone primarily associated with lactation and reproductive function. Monitoring prolactin levels helps diagnose and manage conditions related to fertility, menstrual irregularities, and lactation. Elevated prolactin levels, known as hyperprolactinemia, can disrupt menstrual cycles, leading to irregular periods or absent menstruation (amenorrhea). It may also cause infertility or difficulty conceiving. In men, it can lead to reduced libido and erectile dysfunction. Balanced prolactin levels support reproductive health and hormone regulation.
- DHT (Dihydrotestosterone): DHT is a potent form of testosterone involved in male reproductive function and secondary sexual characteristics. Monitoring DHT levels aids in assessing androgen-related conditions such as male pattern baldness and benign prostatic hyperplasia. High levels of DHT are associated with male pattern baldness (androgenic alopecia) and benign prostatic hyperplasia (BPH), a non-cancerous enlargement of the prostate gland that can cause urinary symptoms such as frequent urination or difficulty urinating. Optimizing DHT levels supports male reproductive health and hormone balance.
- Iron Profile: The iron profile includes various markers such as serum iron, ferritin, and transferrin, which assess iron status in the body. Monitoring the iron profile helps diagnose and manage conditions such as iron deficiency anemia and hemochromatosis. Low iron levels can lead to iron deficiency anemia, characterized by fatigue, weakness, pale skin, shortness of breath, and difficulty concentrating. High iron levels, known as hemochromatosis, can lead to iron overload, causing symptoms such as joint pain, fatigue, abdominal pain, and organ damage. Optimizing iron levels supports red blood cell production, oxygen transport, and overall energy metabolism.
- Lithium: Monitoring lithium levels is essential to ensure therapeutic effectiveness and avoid toxicity. Low lithium levels may result in mood disorders, leading to persistent or worsening symptoms of depression or mania. High lithium levels, or lithium toxicity, can cause symptoms such as nausea, vomiting, diarrhea, tremors, confusion, drowsiness, and, in severe cases, kidney or neurological problems. Proper management of lithium levels helps stabilize mood and manage symptoms of mood disorders effectively.
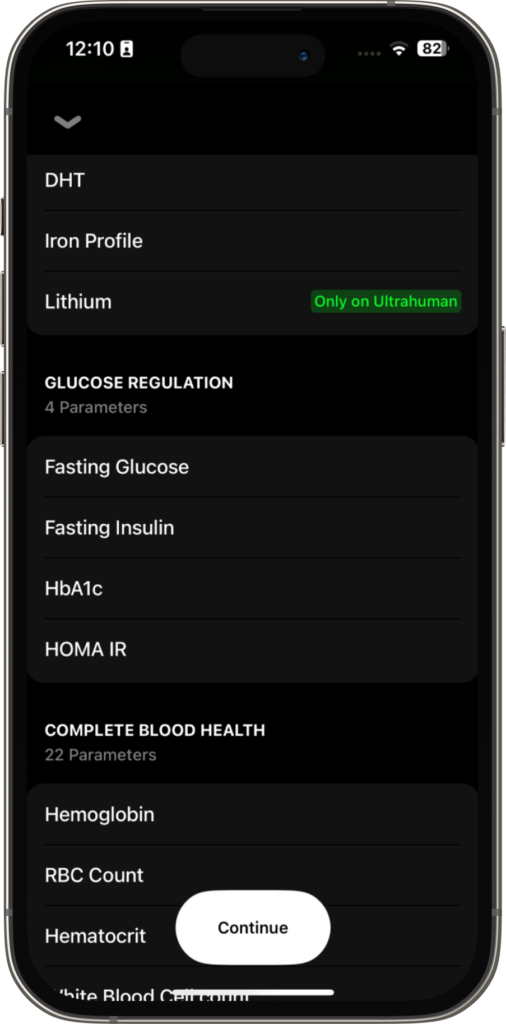
Glucose Regulation
Glucose regulation is vital for maintaining overall health and well-being. Even if you aren’t diabetic or testing for diabetes, this panel is important for you to understand your body and how glucose metabolism happens in your body. The markers in this panel provide insight into how the body processes glucose and its potential impact on health, other than the risk of developing conditions like diabetes. Monitoring and optimizing these parameters support stable energy levels, cognitive function, and overall performance. Here are the blood markers for glucose regulation:
- Fasting Glucose: Fasting glucose levels indicate the concentration of glucose in the blood after an overnight fast. This test is essential as balanced blood glucose levels are crucial for energy production, cognitive function, and overall well-being. Monitoring fasting glucose helps in assessing the body’s ability to regulate blood sugar levels efficiently. Optimizing fasting glucose levels supports stable energy levels, mental clarity, and mood stability, reducing the risk of developing diabetes, fatigue, and cognitive decline, thereby enhancing physical and mental performance.
- Fasting Insulin: Fasting insulin levels assess the body’s insulin response after fasting. Elevated fasting insulin levels may indicate insulin resistance and metabolic dysfunction, which can lead to various health issues, including type 2 diabetes. Monitoring fasting insulin helps in understanding the body’s ability to utilize glucose effectively which is crucial for efficient glucose metabolism, energy stability, and reducing the risk of metabolic diseases, thus supporting overall health and performance.
- HbA1c (Hemoglobin A1c): Measuring HbA1c levels, even if you’re not diabetic, is important for assessing long-term blood sugar control and overall health. Not only does it help early detection of prediabetes and diabetes but it also provides insights into how well your body manages blood sugar over time. By monitoring HbA1c levels, individuals can proactively maintain stable energy, mental clarity, and mood stability, while also reducing the risk of fatigue caused by blood sugar fluctuations and cognitive decline. It’s a valuable tool for optimizing overall physical and mental performance and preventing potential health complications in the future.
- HOMA IR (Homeostatic Model Assessment of Insulin Resistance): HOMA IR calculates insulin resistance based on fasting glucose and insulin levels. This assessment is crucial for identifying early signs of insulin resistance, a precursor to type 2 diabetes and metabolic dysfunction such as PCOS and thyroid. OOptimizing HOMA IR levels is key for enhancing insulin sensitivity, glucose metabolism, and energy utilization, while also supporting hormonal health.

Blood Health Panel
Blood health testing is a cornerstone of maintaining overall well-being and preventing diseases. It offers a window into the body’s physiological functioning, highlighting the efficiency of the immune system, oxygen transportation, and clotting processes. Through the analysis of various blood parameters like red and white blood cell counts, hemoglobin levels, platelet count, and red cell distribution width (RDW), healthcare professionals can pinpoint early signs of imbalance or disease. This proactive approach enables the implementation of targeted interventions to uphold or enhance health. Here’s a concise overview of what’s typically examined in a blood health panel and its relevance:
- RBC (Red Blood Cell) and WBC (White Blood Cell) Counts: These counts are fundamental to assessing overall health and athletic capability. RBCs are pivotal for oxygen delivery to tissues, affecting energy levels and endurance. Anemia, or low RBC count, can cause fatigue and diminished physical stamina. WBCs are the body’s defense against infections, with optimal levels ensuring robust immunity. Regular monitoring of RBC and WBC counts assists in optimizing oxygen transport and immune defense, crucial for sustained health and physical performance.
- Hemoglobin: This protein’s role in transporting oxygen underscores its importance for both vitality and athletic performance. Adequate hemoglobin levels are essential for efficient oxygen delivery to muscles, enhancing endurance and physical output. Conversely, low or high hemoglobin levels might indicate health issues, impacting energy and recovery times. Tracking hemoglobin levels facilitates the fine-tuning of oxygen supply to tissues, supporting peak performance and health.
- Platelet Count and Mean Platelet Volume (MPV): Key for clotting and recovery, platelets help prevent excessive bleeding and are essential for healing post-injury. Adequate platelet levels and functionality are critical for quick recovery, ensuring minimal training interruptions. MPV offers insights into platelet size and activity, relevant for clotting efficiency and wound healing. Maintaining optimal platelet metrics is beneficial for swift recovery from injuries, enhancing training consistency and performance.
- Neutrophils, Lymphocytes, Eosinophils, Basophils: The balance among these white blood cell types reflects overall immune health and capacity. Neutrophils combat bacterial infections; lymphocytes are vital for adaptive immunity; eosinophils and basophils are involved in allergic and inflammatory responses, respectively. Monitoring these cells aids in assessing immune strength and potential vulnerabilities, ensuring athletes can endure the rigors of training and competition by minimizing illness risks.
- Red Cell Distribution Width (RDW): RDW indicates the variability in RBC sizes, with deviations signaling potential health concerns like anemia or nutritional deficiencies. For athletes, consistent RDW values are essential for optimal oxygen delivery and performance endurance. Abnormal RDW can lead to reduced oxygen transport, affecting stamina, exercise tolerance, and recovery. Regular RDW checks help in the early identification of issues, allowing timely corrective actions to support health and athletic achievements.
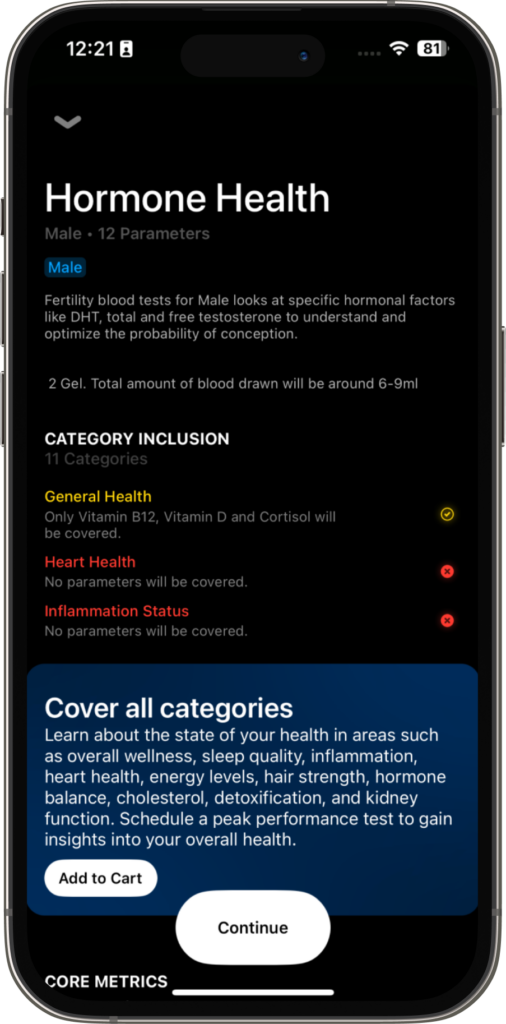
Hormonal Health Panel
Measuring hormone health is crucial for peak performance and overall health as hormones play a vital role in regulating various physiological functions. Optimal hormone levels are essential for maintaining energy levels, muscle mass, bone density, mood stability, immune function, and reproductive health, all of which are critical for achieving peak physical and mental performance. Imbalances or deficiencies in hormones can lead to fatigue, decreased strength and endurance, impaired recovery, mood disturbances, and increased susceptibility to illness, hindering both athletic performance and overall well-being. Regular monitoring of hormone levels allows for early detection of imbalances or deficiencies, enabling timely interventions to optimize hormonal balance and support peak performance and health. Here are the blood markers we measure under this panel:
- Cortisol: Cortisol, a key hormone the adrenal glands produce, plays a vital role in maintaining hormone health and balance. High levels of cortisol over time can lead to thyroid dysfunction, cause menstrual irregularities, and change libido by influencing other hormone-producing glands. Similarly, chronically low cortisol levels can indicate that the adrenal glands are not functioning properly, affecting the overall balance of hormones and impacting the endocrine system’s health. Monitoring and optimizing cortisol levels allow individuals to support their hormone system’s health, ensuring it operates harmoniously, which is essential for physical and mental well-being and resilience against stress.
- Testosterone (free and total): Testosterone, both in its free and total forms, is foundational to hormone health, directly influencing an array of bodily functions and systems. This hormone is integral to maintaining libido, muscle mass, bone density, and emotional well-being. When testosterone levels are too low, it can disrupt the body’s hormonal equilibrium, leading to decreased energy, diminished muscle strength, and slower recovery times after physical activity. On the flip side, excessively high levels of testosterone might also disturb the hormonal balance, manifesting as mood fluctuations, increased aggression, and other health complications. Thus, optimizing testosterone levels is crucial for ensuring the endocrine system’s proper function, supporting not only vitality and physical capabilities but also contributing to a balanced hormonal state essential for overall health and performance.
- Prostate-specific Antigen (PSA), DHEAS: PSA is a marker for prostate health, while DHEAS reflects adrenal function and testosterone precursor levels. Monitoring PSA levels is essential for early detection of prostate issues, including inflammation or cancer, which can impact both health and quality of life. Additionally, DHEAS levels provide insights into adrenal health and hormonal balance, influencing energy levels, libido, and overall vitality. Maintaining optimal levels of these hormones supports prostate health, hormonal balance, and overall well-being, facilitating sustained performance and vitality.
- Estradiol, SHBG (Sex Hormone Binding Globulin): Estradiol and SHBG levels are vital for reproductive health, mood regulation, and metabolic function. Imbalances in estrogen levels may lead to symptoms like mood swings, irregular menstrual cycles, and decreased libido. Similarly, abnormalities in SHBG levels can affect the availability of sex hormones, impacting fertility, bone health, and metabolic function. Monitoring these hormones helps maintain hormonal balance, supporting reproductive health, mood stability, and metabolic function, which are crucial for both health and performance.
- Progesterone, Follicle-stimulating Hormone (FSH), Luteinizing Hormone (LH): Progesterone, FSH, and LH play integral roles in reproductive health, menstrual cycle regulation, and fertility. Imbalances in these hormones can lead to irregular menstrual cycles, difficulty conceiving, and hormonal disturbances. Furthermore, disruptions in reproductive hormone levels may affect mood, energy levels, and overall well-being. Monitoring these hormones helps optimize fertility, menstrual health, and hormonal balance, supporting reproductive function, vitality, and emotional well-being.
- Vitamin B12: Vitamin B12 plays a significant role in hormone health due to its crucial functions in nerve function, DNA synthesis, and red blood cell production. Adequate levels of vitamin B12 are vital for the proper functioning of the endocrine system, as deficiencies can lead to symptoms that indirectly affect hormone regulation, such as fatigue and weakness, which impact energy metabolism and cognitive function. Furthermore, vitamin B12 is integral to the synthesis of certain hormones and neurotransmitters that regulate mood and cognitive function. Regular monitoring and maintaining optimal vitamin B12 levels are essential for supporting the body’s hormonal balance, contributing to optimal nerve function, energy metabolism, and overall hormonal health. This, in turn, is crucial for sustaining performance, vitality, and well-being.
- Vitamin D: Vitamin D plays a crucial role in hormone health, particularly concerning bone strength, immunity, and mood stability. It’s instrumental in regulating essential minerals like calcium and phosphorus, vital for maintaining hormonal balance and bone health. When there’s a shortfall in vitamin D, this balance can be thrown off, potentially leading to weakened bones and heightened susceptibility to mood fluctuations. Interestingly, vitamin D receptors are distributed throughout various body tissues, including those involved in hormone production, indicating its broad-reaching influence on the endocrine system. Regular monitoring to ensure optimal vitamin D levels is essential for upholding hormone health, supporting bone density, fortifying the immune system, and preserving emotional equilibrium. This proactive approach is fundamental for achieving and sustaining overall well-being and peak physical performance.
- TSH (Thyroid-stimulating Hormone): TSH regulates thyroid hormone production, affecting metabolism, energy levels, and body temperature. Imbalances in TSH levels can indicate thyroid disorders such as hypothyroidism or hyperthyroidism, which can impact both health and performance. Hypothyroidism (underactive thyroid gland) may lead to symptoms like fatigue, weight gain, and decreased exercise tolerance, while hyperthyroidism (overactive thyroid gland)can cause symptoms like nervousness, rapid heartbeat, and weight loss. By ensuring the health of the thyroid gland and TSH levels, individuals can better support their hormone health, fostering sustained performance, and vitality in daily life.
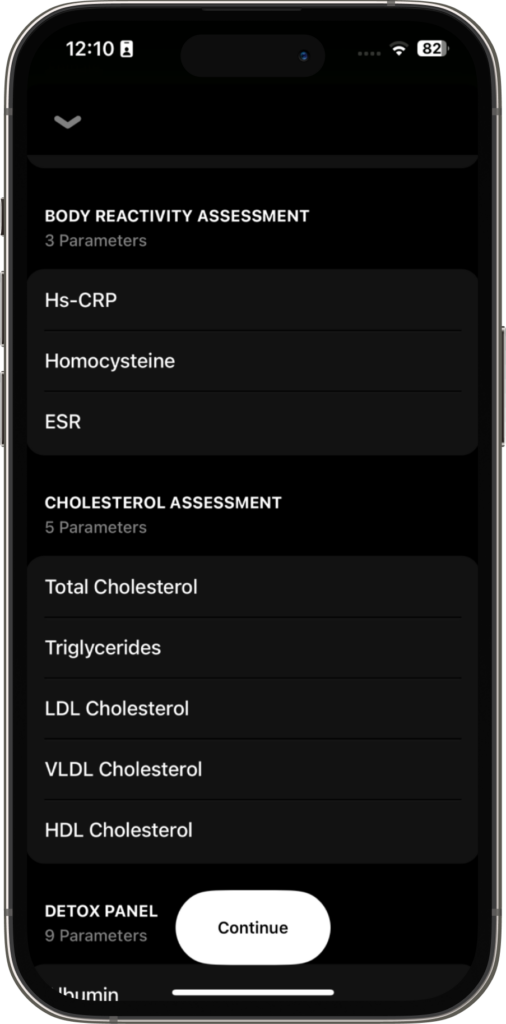
Body Reactivity Assessment
- Hs-CRP (High-Sensitivity C-Reactive Protein): Measuring High-Sensitivity C-Reactive Protein (Hs-CRP) levels is a key component in assessing how our bodies react to various factors, whether they’re physical, emotional, or environmental. Essentially, Hs-CRP tests give us a peek into our body’s inflammatory response system, showing us how it’s dealing with stress, infections, or any kind of injury, as well as potential underlying health issues. Elevated Hs-CRP levels usually signal an increase in inflammation, suggesting that our body is under some type of stress or fighting off something. This kind of assessment is crucial because it provides insight into our overall health and helps us understand the risk of developing chronic conditions. By monitoring and managing inflammation—which can be achieved through lifestyle changes and stress reduction techniques—we’re essentially fine-tuning our body’s responses. This not only promotes better health outcomes but also significantly improves our well-being.
- Homocysteine: Homocysteine, an amino acid regulated by vitamins B12, B6, and folate, serves as a crucial indicator in body reactivity assessments, reflecting more than just cardiovascular health. Elevated levels may hint at broader health risks, including the potential for heart disease, stroke, and even impacts on mental well-being and bone health. For athletes, controlling homocysteine is essential for maintaining heart health and endurance. Elevated levels may affect blood flow and oxygen transport, impacting exercise capacity and overall performance. Lowering homocysteine enhances muscle oxygenation, increases exercise tolerance, and supports sustained high performance.
- ESR (Erythrocyte Sedimentation Rate): In the context of body reactivity assessment, the Erythrocyte Sedimentation Rate (ESR) is a critical indicator that offers insights into inflammation and tissue damage within the body. It’s an essential tool not just for diagnosing and monitoring inflammatory diseases but also for understanding how one’s body responds to stress, injury, or exercise. Particularly for athletes or anyone who keeps fit, a regular check on ESR levels can be a game-changer. It helps in optimizing recovery, reducing injury risks, and tackling issues like muscle soreness and fatigue head-on. By keeping inflammation in check, individuals can improve their recovery time, minimize fatigue, and ensure they are operating at their peak physical potential, making ESR a pivotal part of managing and enhancing body reactivity.
Cholesterol Assessment
Assessing your cholesterol is crucial for multiple reasons, as each component offers distinct insights into cardiovascular wellness, impacting overall health and performance. Monitoring cholesterol levels not only helps in understanding heart health but also guides lifestyle choices and treatment strategies to support physical well-being, cognitive function, and endurance.
- Total Cholesterol: Total Cholesterol measurement gives a comprehensive overview of your cholesterol levels, combining the quantities of LDL, HDL, and other fats in your blood. High total cholesterol can indicate an increased risk for heart disease and stroke. Beyond heart health, total cholesterol levels can offer insights into various aspects of overall wellness. Elevated total cholesterol levels may impact brain health, potentially increasing the risk of cognitive decline and Alzheimer’s disease. Additionally, high cholesterol levels can affect endurance and stamina during physical activity by reducing oxygen delivery to muscles.
- Triglycerides: Elevated triglyceride levels not only pose risks to cardiovascular health but also serve as indicators of broader health concerns. High triglycerides are often associated with metabolic syndrome, fatty liver disease, inflammation, and potentially increased risk of cognitive decline. Monitoring and managing triglyceride levels through lifestyle modifications can therefore have far-reaching implications for overall health and well-being, encompassing metabolic health, liver function, inflammation levels, and brain health beyond cardiovascular wellness.
- LDL (Low-Density Lipoprotein): Elevated LDL, known as “bad” cholesterol, not only pose risks to cardiovascular health but also offer insights into broader health concerns. High LDL cholesterol has been linked to increased risk of cognitive decline, Alzheimer’s disease, inflammation, and liver dysfunction. Monitoring and managing LDL cholesterol levels are crucial not only for maintaining heart health but also for supporting brain function, reducing inflammation, and promoting overall metabolic and liver health.which is essential for sustained physical activity and overall health.
- HDL (High-Density Lipoprotein): Elevated HDL, or “good” cholesterol, not only signifies better cardiovascular health but also correlates with broader wellness markers. High HDL levels are associated with improved cognitive function, reduced inflammation, and enhanced immune response. Furthermore, HDL cholesterol plays a role in maintaining liver health and supports metabolic processes. By boosting HDL levels, individuals can not only mitigate cardiovascular risks but also promote overall well-being, including cognitive health, immune function, liver function, and metabolic balance.
- VLDL (Very Low-Density Lipoprotein): Monitoring VLDL, along with LDL and triglycerides, provides valuable insights beyond cardiovascular health, offering clues about metabolic health, liver function, and inflammation. Elevated VLDL levels may indicate increased risk not only for heart disease but also for metabolic syndrome, fatty liver disease, and inflammatory conditions. By managing VLDL levels through lifestyle and treatment interventions aimed at controlling LDL and triglycerides, individuals can promote overall health and well-being, supporting not only heart health and physical performance but also metabolic balance, liver function, and inflammation levels.
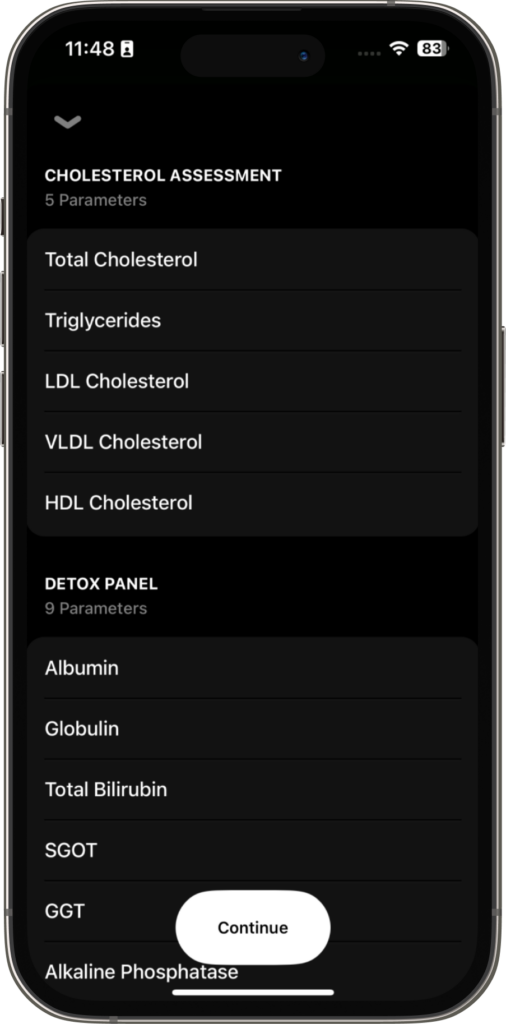
Detox Panel
The detox panel is a set of blood tests used to assess the health and functionality of the liver, an essential organ responsible for detoxification, metabolism, and various other critical processes. Here’s what each marker in the detox panel signifies, why it’s tested, what it can reveal about your health, and how its levels can be optimized for better health and performance:
- Albumin: This is the most abundant protein made by the liver, essential for maintaining fluid balance and transporting hormones, vitamins, and drugs throughout the body. Testing for albumin levels helps assess liver function and nutritional status. Low levels may indicate liver damage or disease. Enhancing albumin can involve improving overall nutrition, particularly protein intake, and addressing any underlying liver conditions.
- Globulin: Globulin is a group of proteins involved in immune response, clotting, and other functions. The globulin test, often part of the total protein measurement, can indicate immune system health and liver function. Abnormal levels may suggest liver or kidney disorders, or immune diseases. Maintaining healthy globulin levels typically involves ensuring adequate nutrition and managing any underlying health conditions affecting the liver or immune system.
- Total Bilirubin: Bilirubin is a waste product from the breakdown of red blood cells, processed by the liver. High levels can indicate liver dysfunction or other conditions affecting red blood cell breakdown. Testing for total bilirubin helps in diagnosing jaundice and assessing liver health. Keeping bilirubin levels in check involves managing liver health through diet, avoiding excessive alcohol consumption, and addressing any liver or gallbladder diseases.
- SGOT (AST) and SGPT (ALT): These enzymes are found in the liver and other tissues. Elevated levels can indicate liver damage or disease. Testing for SGOT and SGPT helps in detecting liver injury and monitoring liver health. Reducing elevated enzyme levels involves lifestyle changes such as reducing alcohol intake, maintaining a healthy weight, and managing conditions like hepatitis or fatty liver disease.
- GGT (Gamma-Glutamyl Transferase): This enzyme is involved in bile formation and is another marker of liver health. High GGT levels may indicate liver disease, alcohol abuse, or bile duct problems. Testing for GGT helps in diagnosing and monitoring these conditions. Improving GGT levels can include reducing alcohol consumption, losing weight if overweight, and treating underlying liver conditions.
- Alkaline Phosphatase: This enzyme is related to bile ducts and bone health. Elevated levels can indicate liver or bone disorders. Testing for alkaline phosphatase assists in diagnosing liver, gallbladder, or bone diseases. Managing alkaline phosphatase levels might involve addressing the underlying condition causing the elevation, such as liver disease or bone disorders.
- Direct and Indirect Bilirubin: These tests differentiate between bilirubin directly processed by the liver (direct) and unprocessed bilirubin (indirect). High levels of direct bilirubin can indicate liver dysfunction, while high indirect levels may suggest problems with red blood cell breakdown. Managing bilirubin levels involves improving liver health through lifestyle changes and addressing specific diseases affecting the liver or red blood cells.

Micronutrients
Micronutrients play essential roles in bodily functions, and their levels can offer insights into overall health, nutrient deficiencies, and potential health issues. Testing for these markers can help tailor dietary and supplementation plans to improve health and performance.
- Ferritin: Reflecting the body’s iron stores, ferritin levels are key for diagnosing iron status. Adequate ferritin is essential for optimal oxygen transport and energy levels and is crucial for maintaining endurance and mental sharpness. For peak performance, ensuring proper iron levels through diet or supplements is vital, with an emphasis on managing intake to avoid deficiency (which can lead to anemia and decreased performance) or overload (which may cause organ damage).
- Vitamins B1 (Thiamine), B2 (Riboflavin), B6, B9 (Folate), and B12: These B vitamins are fundamental for energy production, brain health, and cell repair, directly impacting physical performance and cognitive function. Deficiencies can result in fatigue, compromised immune function, and reduced muscle recovery, hindering performance. A diet rich in these vitamins supports energy levels and neurological health, critical for athletes and active individuals seeking to optimize performance and recovery.
- Vitamin D: Beyond its role in bone health, Vitamin D is pivotal for immune function and mood regulation, influencing both health and athletic performance. Optimal levels contribute to muscular strength, reduced inflammation, and enhanced recovery. For individuals aiming for peak performance, maintaining Vitamin D through sun exposure, diet, and possibly supplementation is key to supporting muscle function and immune resilience.
- Calcium: As a vital mineral for bone strength and cellular function, calcium’s importance extends to muscle contraction and nerve signaling, affecting athletic performance and exercise capacity. Adequate calcium intake, through diet or supplements, ensures bone density and muscular function are maintained, crucial for high-impact activities and overall health.
- Magnesium: Supporting over 300 enzyme reactions, magnesium’s role in muscle function, nervous system health, and energy metabolism directly affects physical performance and recovery. Low levels can impair muscle function and energy levels. Including magnesium-rich foods in the diet supports optimal muscle and nervous system health, enhancing performance and recovery.
- Iron: Essential for hemoglobin production and effective oxygen transport, iron is crucial for maintaining energy levels and endurance. Iron deficiency can lead to fatigue and impaired performance, while excess iron may cause health issues. Balancing iron intake through diet or supplements is vital for optimal physical performance, especially for endurance athletes who need efficient oxygen delivery to maintain their activity levels.
Muscle Health Panel
Measuring muscle health through specific tests is crucial for gauging physical performance and maintaining overall wellness. These evaluations reveal the state of muscles and tissues, uncovering potential issues that could hinder peak performance or everyday health. Regular integration of these tests into health check-ups or performance assessments enables proactive steps toward preventing injuries, ensuring efficient recovery, and achieving optimal physical capabilities. The key markers for assessing muscle health include:
- CPK (Creatine Phosphokinase): A marker of muscle health, CPK levels elevated in response to muscle damage. High CPK can indicate injuries, effects of intense exercise, or conditions like overtraining and muscle diseases. Monitoring CPK helps in tailoring training to allow sufficient recovery and prevent overexertion. Strategies to manage CPK for improved muscle health involve incorporating rest days, focusing on a muscle-supportive diet, and using recovery techniques like stretching and hydration.
- LDH (Lactate Dehydrogenase): LDH levels, which increase with cellular or tissue damage, provide insights into overall tissue health, including muscle tissue. Elevated LDH can signal overexertion, recovery status, or more severe health issues. Adjusting training intensity, enhancing recovery practices, and optimizing nutrition based on LDH levels can support tissue health, injury prevention, and peak performance. A balanced diet, rest, and careful exercise planning are essential for managing LDH levels and promoting tissue regeneration and growth.
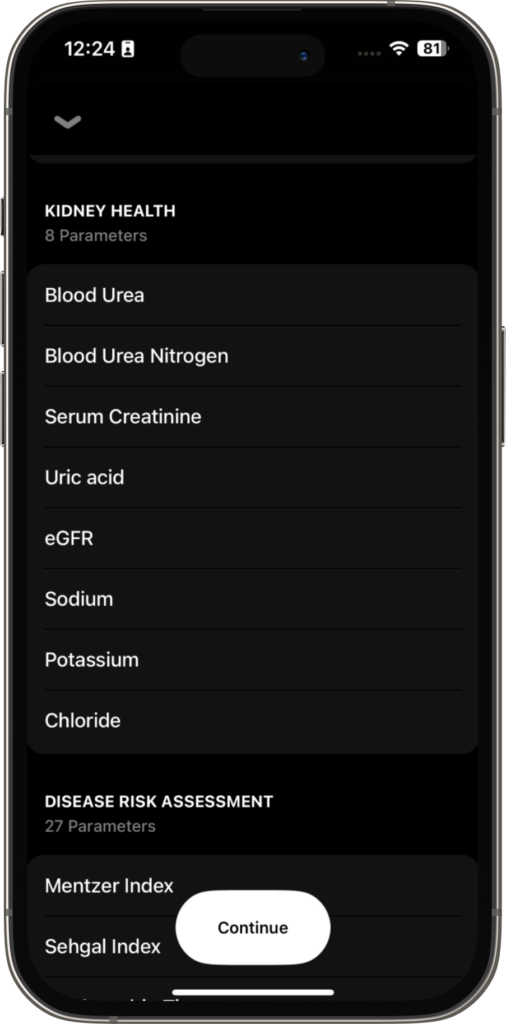
Kidney Health Panel
Kidney health is fundamental to overall wellness and optimal physical performance, as kidneys play a crucial role in filtering waste, maintaining electrolyte balance, and regulating blood pressure. Various blood markers can provide insights into kidney function, highlighting potential issues and guiding interventions to preserve or enhance renal health and support athletic performance. Here’s an overview of key kidney health markers:
- Blood Urea & Blood Urea Nitrogen (BUN): Urea is a waste product formed during protein breakdown, and BUN measures the amount of nitrogen in the blood that comes from urea. It directly assesses your renal health. Elevated levels can indicate kidney dysfunction or dehydration, as kidneys are responsible for filtering urea from the blood. High BUN levels might suggest compromised kidney function or a diet too high in protein for the kidneys to process efficiently. For athletes, maintaining optimal BUN levels is crucial for recovery and performance, as it reflects the body’s ability to eliminate waste and manage hydration. Adequate hydration, adjusting protein intake, and managing blood pressure can support kidney health and optimize BUN levels.
- Uric Acid: Uric acid is produced from the breakdown of purines found in certain foods. High levels can lead to kidney stones and gout, indicating that the kidneys are not filtering uric acid effectively. For individuals aiming for peak performance, managing uric acid levels is essential to prevent joint pain and ensure efficient waste elimination, contributing to better recovery and endurance. A diet low in purines, increased water intake, and possibly medications can help manage uric acid levels.
- Electrolytes (Sodium, Chloride, Potassium): These minerals are vital for fluid balance, muscle function, and nerve signaling. Imbalances can indicate kidney dysfunction, as kidneys regulate these electrolytes in the body. Optimal electrolyte balance is crucial for athletes to maintain hydration, muscle strength, and overall performance. A balanced intake of electrolytes through diet, staying hydrated, and monitoring with sports drinks or supplements as needed, especially during prolonged physical activity.
- eGFR (Estimated Glomerular Filtration Rate): eGFR is a calculation based on creatinine levels, age, race, and gender, estimating how well the kidneys are filtering waste. It’s the best overall indicator of kidney function, with low values suggesting impaired kidney health. Maintaining a healthy eGFR is essential for anyone, especially athletes, as efficient waste filtration supports recovery, energy levels, and overall health. Regular monitoring, maintaining a healthy diet, managing conditions like hypertension and diabetes, and avoiding substances harmful to the kidneys can help maintain or improve eGFR.
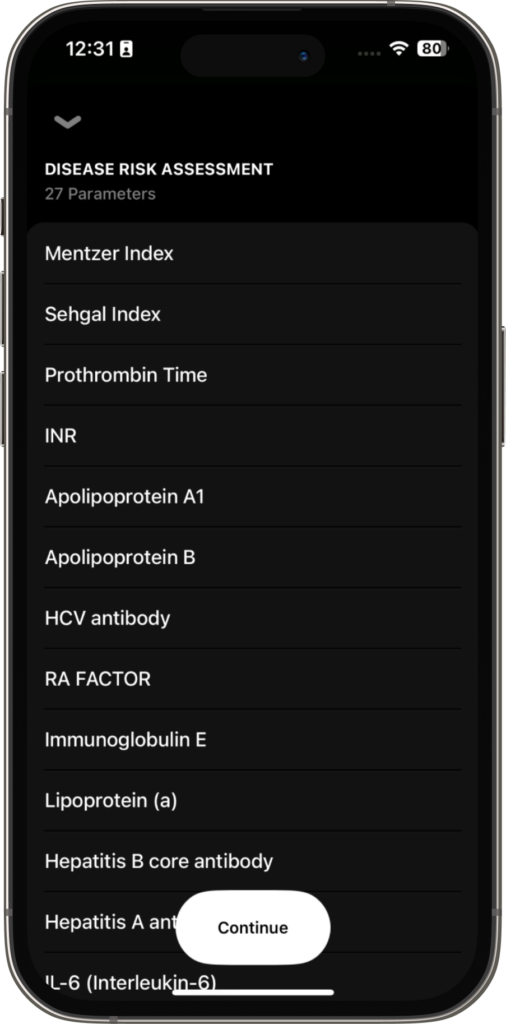
Diseases Risk Assessment
Disease risk assessment through blood tests provides critical insights into an individual’s health status, highlighting areas of concern and guiding preventive strategies. Here’s a breakdown of several key markers and their importance:
- Apolipoprotein A1 and B: These proteins are crucial components of HDL (“good”) and LDL (“bad”) cholesterol, respectively. Apolipoprotein A1 is associated with a reduced risk of cardiovascular disease as it helps to remove cholesterol from the bloodstream, while Apolipoprotein B is linked to a higher risk due to its role in transporting cholesterol to tissues, potentially leading to plaque buildup. While Apolipoprotein A1 and B are primarily associated with cardiovascular disease risk, their levels may also have implications for other health conditions. For instance, higher levels of Apolipoprotein B have been linked to an increased risk of metabolic syndrome, a cluster of conditions that includes high blood pressure, high blood sugar, abnormal cholesterol levels, and excess abdominal fat, all of which elevate the risk of heart disease, stroke, and type 2 diabetes.
- Hepatitis B, A, and E Antibody: Testing for antibodies against these viruses can indicate past or present infections, providing essential information on liver health and immune status. Since hepatitis can significantly impact liver function and athletic performance, identifying exposure or immunity allows for targeted interventions, including vaccination or treatment, to protect liver health and maintain peak performance.
- TIBC (Total Iron Binding Capacity) and UIBC (Unsaturated Iron Binding Capacity): These tests measure the blood’s capacity to bind and transport iron, offering insights into iron metabolism and potential anemia risk. Since iron is crucial for oxygen transport and energy production, understanding TIBC and UIBC can help in diagnosing iron deficiency or overload, informing dietary adjustments or supplementation to support optimal health and athletic performance.
- Immunoglobulin E (IgE): Elevated IgE levels can indicate allergic conditions or parasitic infections, affecting overall well-being and performance. High IgE levels may lead to allergic reactions or asthma, impairing exercise capacity. Identifying high IgE can guide dietary modifications, environmental changes, or medical interventions to manage allergies and enhance physical capabilities.
- Lipoprotein (a) [Lp(a)]: Lp(a) is a lipoprotein associated with an increased risk of cardiovascular diseases. Unlike other cholesterol markers, Lp(a) levels are largely determined by genetics. High Lp(a) can be an independent risk factor for heart disease, guiding more aggressive prevention strategies in individuals with elevated levels to manage heart health and ensure long-term performance sustainability.
- Iron: Essential for hemoglobin production and oxygen transport, iron levels are critical for energy, cognitive function, and endurance. Testing for iron can diagnose deficiency or overload, both of which can detrimentally affect health and performance. Appropriate iron levels can be maintained through diet or supplementation, ensuring optimal oxygen delivery to tissues and supporting vigorous physical activity.
- Alpha 1, Alpha 2, Beta 1, Beta 2, Gamma Globulin: These serum proteins play various roles in the body, including clotting, transport, and immune response. Abnormal levels can indicate a range of health issues from liver disease to immune disorders. Understanding these levels can help diagnose underlying conditions early, enabling interventions that preserve health and athletic ability, and highlighting the interconnectedness of protein balance, immune function, and overall physical performance.

Thyroid Health Panel
Thyroid health is paramount for metabolic regulation, energy levels, and overall physiological balance, affecting both everyday well-being and peak performance. Understanding thyroid function through specific markers can guide interventions to optimize health and performance.
- Free T3 and T4: Triiodothyronine (T3) and Thyroxine (T4) are hormones produced by the thyroid gland, playing vital roles in metabolism, heart rate, and temperature regulation. The “free” forms of these hormones (Free T3 and T4) are unbound and active in the body. Testing for these provides insights into the thyroid’s functionality; abnormalities can indicate hyperthyroidism (excess hormones) or hypothyroidism (hormone deficiency). Both conditions can impact energy levels, recovery, and metabolic rate, crucial for physical performance. Managing optimal levels often involves dietary adjustments, lifestyle changes, or thyroid hormone replacement therapy, aiming to stabilize metabolic rate and energy levels for enhanced performance and health.
- TSH (Thyroid-Stimulating Hormone): TSH, produced by the pituitary gland, regulates the production of thyroid hormones by stimulating the thyroid gland. It’s a key indicator of thyroid health; elevated TSH levels typically suggest hypothyroidism, while low levels may indicate hyperthyroidism. Testing for TSH is crucial for diagnosing thyroid disorders early, allowing for interventions that can mitigate symptoms like fatigue, weight changes, and impaired performance.
- Anti-TPO (Thyroid Peroxidase Antibodies): Anti-TPO antibodies target thyroid peroxidase, an enzyme crucial for thyroid hormone production. High levels can indicate autoimmune thyroid diseases such as Hashimoto’s thyroiditis (leading to hypothyroidism) or Graves’ disease (which can cause hyperthyroidism). Testing for Anti-TPO helps in diagnosing these autoimmune conditions, guiding treatment plans that may include immunomodulatory strategies, lifestyle modifications, or hormone therapy, aiming to maintain energy levels and metabolic health for optimal performance.
- Anti-TG (Thyroglobulin Antibodies): Anti-TG antibodies target thyroglobulin, a protein involved in thyroid hormone production. Like Anti-TPO, elevated Anti-TG levels are often associated with autoimmune thyroid conditions. Identifying high Anti-TG levels can assist in confirming diagnoses and tailoring treatments to manage or mitigate the impact of thyroid autoimmunity on health and athletic performance, ensuring that thyroid health supports rather than hinders physical activity and recovery.
Conclusion
Understanding your body through the lens of blood markers is a transformative approach to achieving peak health and performance. By leveraging Blood Vision and the Peak Performance Test, you’re equipped with the tools to decode the complexities of your wellness and fine-tune your lifestyle for optimal health. These innovative assessments provide a comprehensive overview of crucial health parameters, from heart health and inflammation to thyroid function and micronutrient levels, guiding personalized interventions. Embrace this journey with our app, where Blood Vision and the Peak Performance Test await to unlock your full potential, blending cutting-edge science with personalized health strategies to empower you towards achieving and maintaining your best self.